Off-Label Prescription Coverage Estimator
Why Coverage Matters
Only 45% of off-label prescriptions are covered by insurance. This tool estimates your likelihood of coverage based on key factors from the article.
Enter your details above to see your coverage estimate.
Every year, millions of people in the U.S. take medications that weren’t officially approved by the FDA for their specific condition. That’s not a mistake. It’s not illegal. And in many cases, it’s the best option they have. This is called off-label drug use-when a doctor prescribes a drug for a purpose, age group, dose, or route that hasn’t been formally approved by regulators. It’s common, often necessary, and sometimes life-saving. But it’s also risky, confusing, and rarely talked about in plain terms.
What Exactly Is Off-Label Use?
When the FDA approves a drug, it’s based on data from clinical trials showing the drug works safely for a specific condition-say, treating high blood pressure or rheumatoid arthritis. But once that drug is on the market, doctors can legally prescribe it for anything they believe will help their patient. That’s because the FDA regulates what drug companies can sell, not how doctors practice medicine. Off-label use falls into four main categories:- Using a drug for a different disease (e.g., using a chemotherapy drug approved for breast cancer to treat ovarian cancer)
- Giving it in a different way (e.g., swallowing a pill meant to be injected)
- Changing the dose (e.g., doubling the approved amount)
- Prescribing it for a group not studied (e.g., giving adult medications to children)
It’s not rare. Around 20% of all prescriptions in the U.S. are off-label. In pediatrics, it’s even higher-62% of prescriptions for kids are off-label because most drugs were never tested on children. In oncology, up to 85% of cancer drugs are used off-label. In psychiatry, nearly one in three prescriptions falls outside the label.
Why Do Doctors Do It?
The answer is simple: sometimes, there’s no other choice. Take methotrexate. It was approved for cancer and psoriasis. But doctors discovered it also works for rheumatoid arthritis, Crohn’s disease, and even ectopic pregnancies. Today, those are some of its most common uses-none of which were in the original FDA approval. Or consider antipsychotics like quetiapine. Approved for schizophrenia and bipolar disorder, they’re now routinely prescribed for insomnia, anxiety, and even dementia-related agitation-despite limited evidence and serious side effects like weight gain and diabetes risk. In pediatrics, it’s often the only option. Fewer than 30% of drugs have pediatric labeling. A child with a rare seizure disorder might get a drug approved only for adult epilepsy because it’s the only one that’s shown any effect. Waiting for formal approval could take years-or never happen. Oncology is another big driver. Cancer isn’t one disease. It’s hundreds. A drug that targets a specific genetic mutation might work across multiple cancer types-even if it was only tested in one. That’s why drugs like trastuzumab (Herceptin) are used for HER2-positive breast, stomach, and even lung cancers, even when only breast cancer was on the label.When Off-Label Use Goes Wrong
It’s not all good news. Off-label use carries real dangers. The most infamous example is Fen-Phen. In the 1990s, doctors prescribed fenfluramine and phentermine together for weight loss-even though neither was approved for that use. The combination caused severe heart valve damage. Thousands were injured. The drugs were pulled from the market. It’s a textbook case of how off-label use, without strong evidence, can become a public health disaster. Even today, drugs like semaglutide (Ozempic) are being prescribed off-label for weight loss at skyrocketing rates. The FDA approved it for type 2 diabetes. But now, millions are taking it to lose weight-with little long-term safety data for that use. Side effects like nausea, pancreatitis, and gallbladder disease are real. And since it’s off-label, insurance often won’t cover it, leaving patients to pay hundreds per month out of pocket. The problem isn’t just the drug. It’s the lack of warning. When a drug is used off-label, the patient information leaflet doesn’t mention the new use. The pharmacist doesn’t know. The patient might not even realize they’re taking it for something unapproved. That’s why many people don’t know they’re at risk until it’s too late.
Who Pays for It?
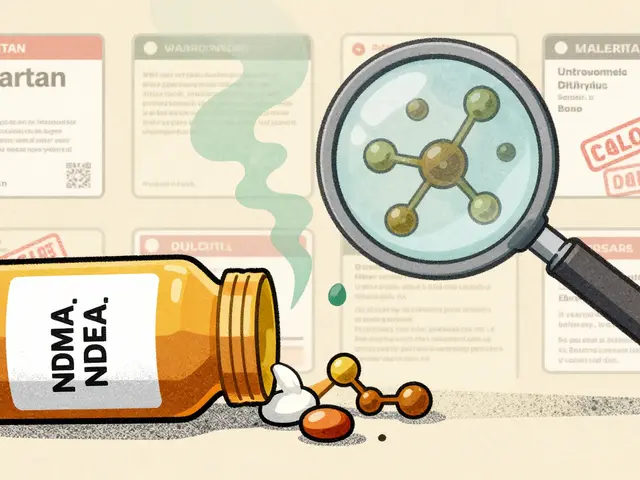
Insurance companies don’t like off-label use. And they don’t have to cover it. Most insurers, including UnitedHealthcare and Medicare, only pay for off-label prescriptions if they’re supported by strong evidence-like peer-reviewed studies, inclusion in the National Comprehensive Cancer Network (NCCN) compendium, or FDA-recognized guidelines. For cancer drugs, this often works. For psychiatric or pediatric uses? Not so much. One oncologist on Reddit shared that she had to fight insurance for prior authorization every time she prescribed vincristine off-label for a rare sarcoma-even though multiple studies showed better outcomes. Each approval took weeks. Delays can cost lives. Patients often end up paying out of pocket. Or they go without. A 2023 study found that 45% of physicians reported off-label prescriptions were delayed by 3 to 5 days because of insurance hurdles. That’s not just frustrating. It’s dangerous.The Legal Line: What Drug Companies Can’t Do
Here’s the twist: while doctors can prescribe off-label, drug companies can’t promote it. It’s illegal for pharmaceutical reps to tell doctors, “This drug works great for insomnia,” if that’s not on the label. They can’t hand out brochures, sponsor educational events, or even mention off-label uses in sales pitches. Violations come with massive fines. GlaxoSmithKline paid $3 billion in 2012 for promoting Paxil for unapproved uses in children and promoting Wellbutrin for weight loss and sexual dysfunction. Pfizer paid $2.3 billion in 2012 for pushing Bextra for off-label heart surgery use. The FDA doesn’t stop off-label use. It stops companies from encouraging it. That’s why so many off-label uses happen quietly-through medical journals, conferences, and word of mouth among doctors.How Do Doctors Decide?
Not all off-label use is equal. Some is backed by solid science. Some is based on guesswork. Good off-label prescribing follows a clear path:- Is there published evidence? (Randomized trials, systematic reviews)
- Is it in a trusted compendium? (NCCN, DRUGDEX, or Off-Patent Drugs Database)
- Is it widely accepted by experts? (Guidelines from the American College of Physicians or ASCO)
- Is the risk worth it? (Are there safer, approved alternatives?)
Doctors who do it right spend time researching. One 2023 study found they spend an average of 27 minutes per patient just to justify an off-label prescription. That’s not just paperwork. It’s clinical judgment.
They also document everything. The American Medical Association says doctors must clearly write down why they chose an off-label use-what evidence they relied on, what alternatives were considered, and what risks the patient was told.
That’s not bureaucracy. That’s protection-for the patient and the doctor.
The Future: Real-World Evidence and Faster Approvals
The system is changing. The 21st Century Cures Act of 2016 gave the FDA new power to use real-world data-like electronic health records and patient registries-to approve new uses faster. Imagine this: thousands of patients take a drug off-label for migraines. Their doctors record outcomes. Over time, patterns emerge. The FDA reviews the data. The drug gets approved for migraines. No new trial needed. That’s the goal. The FDA’s 2023 draft guidance on real-world evidence is a step toward that. It could turn what’s now off-label use into approved treatment in half the time. But it won’t eliminate off-label prescribing. Why? Because medicine isn’t a checklist. It’s a living science. New discoveries happen every day. Rare diseases still lack treatments. Children still need options. And sometimes, the only drug that works is the one not on the label.What Patients Should Know
If your doctor prescribes a drug off-label, here’s what to ask:- Is this approved for my condition? If not, why are you recommending it?
- What studies support this use? Can I see them?
- Are there approved alternatives? What are the risks and benefits of each?
- Will insurance cover it? If not, how much will I pay?
- What side effects should I watch for, even if they’re not listed on the bottle?
Don’t assume off-label means experimental. It often means proven-but not yet officially labeled. And don’t assume it’s unsafe. Many life-saving treatments started as off-label uses.
But do insist on transparency. Your doctor should be able to explain why they chose this drug, not just say, “It’s what we do.”
Off-label prescribing isn’t a loophole. It’s a lifeline. But like any powerful tool, it needs care, evidence, and honesty to be used right.


Chris Clark
December 20, 2025 AT 14:30Man, I had no idea like 20% of all scripts are off-label. My grandma’s arthritis med was one of those-doc just said ‘it works better than the fancy stuff’ and I didn’t question it. Turns out she’s been on methotrexate for 12 years like it’s aspirin.
Nancy Kou
December 22, 2025 AT 09:53This is why we need better real-world data collection. The FDA’s stuck in the 90s. If we tracked outcomes from off-label use like we track social media trends, we’d approve life-saving uses in months, not decades.
Janelle Moore
December 23, 2025 AT 05:45They’re hiding something. Why else would they ban drug companies from talking about it but let doctors do it? Big Pharma is running a secret experiment on us. I’ve seen the reports-people getting sick after taking these ‘off-label’ pills and no one gets held accountable.
Henry Marcus
December 23, 2025 AT 15:12Wait-so the FDA lets doctors gamble with our lives… but if a pharma rep says ‘this might help your insomnia,’ they get fined $2 BILLION? That’s not regulation-that’s a corporate protection racket. The whole system’s rigged. I’m not taking another pill until they admit they’re playing god with our bodies.
Frank Drewery
December 25, 2025 AT 03:02My cousin’s kid has a rare seizure disorder. They tried every approved drug. Nothing worked. Then the neurologist said, ‘Let’s try this one-it’s off-label, but here’s the data.’ Two weeks later, seizures dropped 80%. I’m not mad. I’m grateful.
Ryan van Leent
December 26, 2025 AT 01:52Sajith Shams
December 27, 2025 AT 05:07Off-label use is not medicine. It’s improvisation. In India, we don’t have the luxury of waiting for FDA approval. We use what works. But you Americans act like this is some scandal. It’s not. It’s survival. You’re just scared of what you don’t control.
Adrienne Dagg
December 28, 2025 AT 21:51OMG I JUST REALIZED MY ANTI-DEPRESANT IS OFF-LABEL FOR ANXIETY 😱 I’M SO GLAD I READ THIS. NOW I’M GOING TO ASK MY DOCTOR FOR THE STUDIES. THANK YOU FOR THIS POST!! 🙏
Chris Davidson
December 30, 2025 AT 15:24Off-label prescribing is a symptom of systemic failure. Regulatory stagnation. Inadequate pediatric research. Insurance disincentives. The solution is not to normalize the exception but to fix the system.
Glen Arreglo
January 1, 2026 AT 14:38My oncologist explained everything. Gave me the papers. Said the drug was approved for lung cancer but worked better on mine because of the mutation. Insurance denied it twice. We appealed. Third time, they approved. Took 47 days. I was lucky. Others aren’t.
benchidelle rivera
January 2, 2026 AT 17:05If you're a parent of a child with a rare disease, off-label prescribing isn't a policy debate-it's your child's only shot. I've sat in clinic rooms watching doctors cry because they can't get insurance to cover a drug that might save their patient. This isn't about legality. It's about humanity.
holly Sinclair
January 3, 2026 AT 22:55It’s fascinating how the law treats knowledge as a commodity. The FDA doesn’t regulate practice, only promotion-so the real power lies not with regulators, but with the invisible network of medical journals, conference talks, and whispered recommendations among colleagues. The truth is out there, but only if you know where to look. And if you’re poor, or uneducated, or in a rural town? You’re left guessing. That’s not medicine. That’s epistemic inequality.
Monte Pareek
January 5, 2026 AT 02:28Look I’ve been prescribing off-label for 18 years. I’ve seen people live who would’ve died waiting for approval. But I also know the risks. I don’t just grab a drug off the shelf. I check NCCN. I check UpToDate. I print out the studies. I sit with the patient. I tell them exactly what we know and what we don’t. It takes time. But it’s worth it. This isn’t cutting corners. It’s doing the job right when the system fails.
Kelly Mulder
January 5, 2026 AT 20:24It is rather astonishing, nay, profoundly disconcerting, that the American medical establishment has normalized what is, in essence, an unregulated pharmaceutical experiment conducted on the populace under the guise of clinical discretion. One cannot help but wonder whether this is the inevitable consequence of a healthcare system that prioritizes profit over patient safety. The lack of transparency, the insurance denials, the absence of informed consent protocols-it is, frankly, a travesty.