For years, fish oil supplements have been marketed as a simple fix for a healthy heart. You’ve probably seen the ads: swallow a couple of pills, lower your triglycerides, and protect yourself from heart attacks. But here’s the truth-fish oil isn’t the miracle pill everyone thought it was. The science is messy, contradictory, and changing fast. If you’re taking it hoping to prevent heart disease, you need to know what the latest studies actually say-and who might still benefit.
What Exactly Are Omega-3s?
Omega-3 fatty acids are a type of fat your body can’t make on its own. That means you have to get them from food or supplements. The two most important ones for your heart are EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). They’re found mostly in fatty fish like salmon, mackerel, sardines, and herring. Some plant sources, like flaxseeds and walnuts, contain ALA, a different kind of omega-3 your body can only convert to EPA and DHA in tiny amounts-so don’t count on them for heart protection.
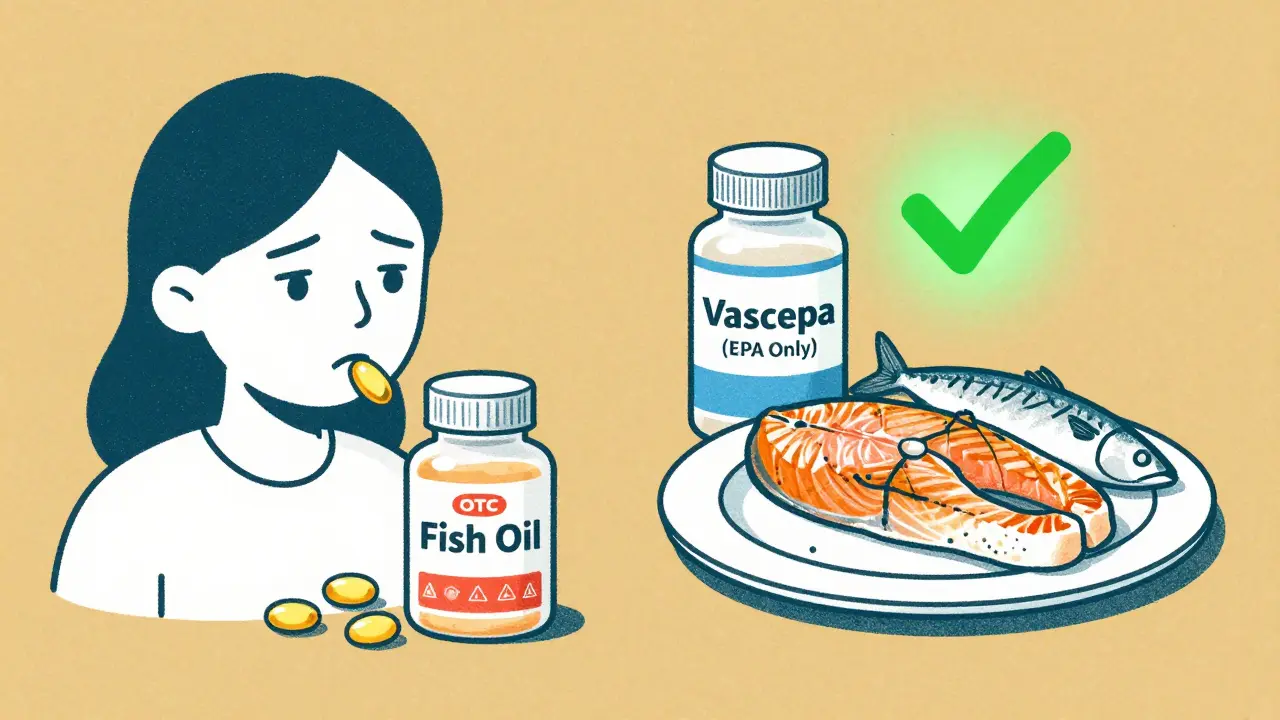
Most fish oil capsules contain both EPA and DHA. But here’s where things get tricky: not all omega-3s work the same way. A high-dose, purified EPA-only prescription drug called icosapent ethyl (brand name Vascepa) showed strong results in one major study. But when researchers tested a mix of EPA and DHA at the same dose, the benefits vanished. That’s not a small detail-it’s the difference between a proven therapy and a placebo.
The Big Studies That Changed Everything
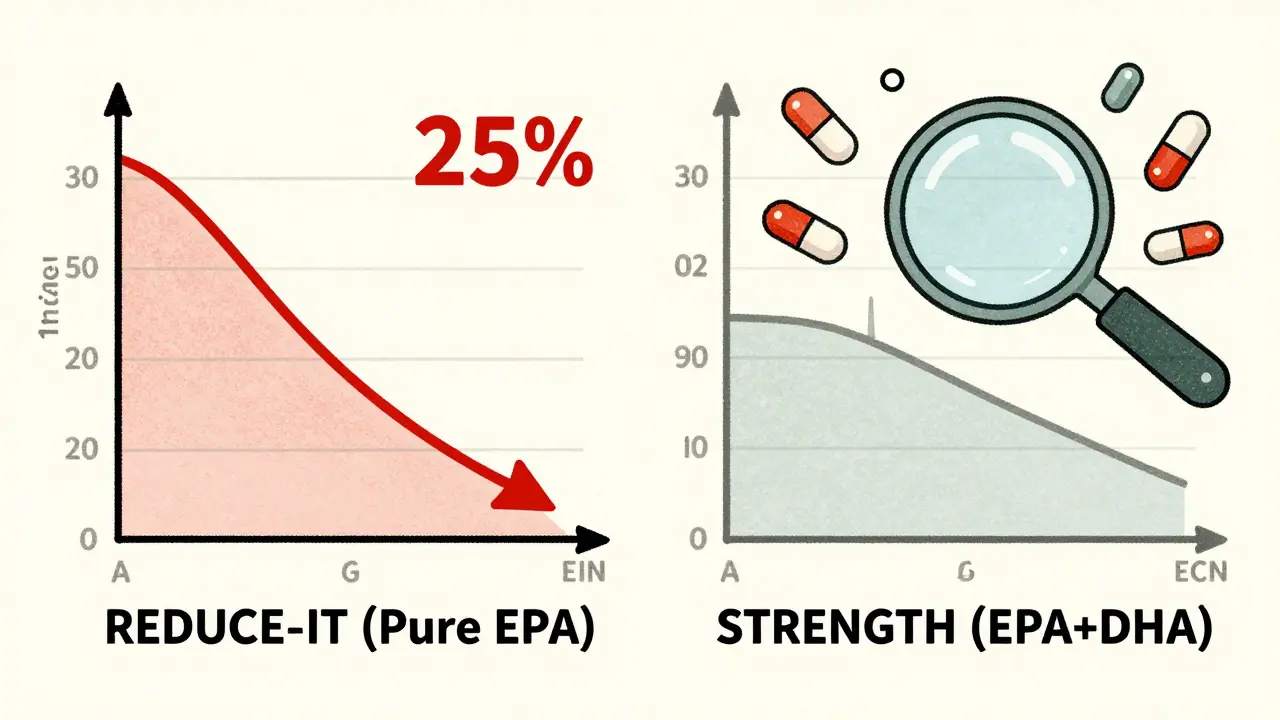
In 2018, the REDUCE-IT trial shocked the medical world. It followed nearly 8,200 people at high risk for heart disease-most were already on statins, with high triglycerides and other risk factors. They were given 4 grams of pure EPA daily. After nearly five years, those taking EPA had 25% fewer heart attacks, strokes, and heart-related deaths. That’s a big deal. The FDA approved Vascepa in 2020 specifically for this use.
But then came STRENGTH in 2020. This trial used the same 4-gram daily dose-but with a mix of EPA and DHA. The results? Nothing. No benefit. The trial was stopped early because it was clear it wouldn’t work. Why the difference? Scientists think DHA might cancel out some of EPA’s benefits. Or maybe it’s the formulation-Vascepa is an ethyl ester, while STRENGTH used a carboxylic acid form. The exact reason isn’t settled, but the message is clear: not all fish oil is created equal.
Then there’s the 2023 Cochrane review-the most comprehensive analysis ever done. It looked at 79 studies with over 112,000 people. The conclusion? Long-chain omega-3 supplements (EPA and DHA) have little to no effect on heart attacks, strokes, or death from heart disease in the general population. That includes people taking standard over-the-counter fish oil pills-usually 300 to 500 mg of EPA/DHA per capsule. If you’re healthy and just popping two pills a day hoping to stay safe, the odds are you’re wasting your money.
Who Might Still Benefit?
Just because fish oil doesn’t help everyone doesn’t mean it helps no one. There are specific groups where the evidence still supports use.
- People with very high triglycerides (over 500 mg/dL): Prescription omega-3s like Lovaza or Vascepa are FDA-approved for this. They can cut triglycerides by 25-30%. That’s important because extremely high levels raise your risk of pancreatitis.
- People who’ve had a heart attack and still have high triglycerides: If you’re on a statin but your triglycerides stay above 135 mg/dL, Vascepa may reduce your chance of another heart event.
- African Americans: The VITAL trial found omega-3 supplements cut heart attacks by 77% in this group. Researchers think genetic differences in how the body processes omega-3s might explain why.
- People with heart failure: The American Heart Association says omega-3s may reduce deaths in this group, though the benefit is modest-around 10%.
For everyone else? The data doesn’t support routine use. That includes healthy people, those with normal cholesterol, or even people with mild high blood pressure. Don’t assume more is better. Taking 1,000 mg of fish oil daily won’t lower your risk if you’re not in one of these high-risk groups.
Prescription vs. Over-the-Counter: Know the Difference
There’s a huge gap between what you buy at the drugstore and what your doctor prescribes.
Over-the-counter fish oil supplements usually contain 300-500 mg of EPA and DHA combined per capsule. To match the dose used in REDUCE-IT, you’d need to take 8-10 capsules a day. That’s expensive, hard to swallow, and risky. Many of these products aren’t tightly regulated. In 2023, Consumer Reports tested 35 brands and found 12 of them had oxidation levels higher than international safety limits. That means the oil could be rancid-losing its potency and possibly causing inflammation instead of reducing it.
Prescription omega-3s like Vascepa and Lovaza are pure, tested, and standardized. Vascepa contains only EPA, and it’s been proven to reduce heart events. Lovaza has EPA and DHA but is only approved for triglycerides over 500 mg/dL-not for preventing heart attacks. These cost $300 a month, even with insurance. Most insurers only cover them for specific, documented conditions.
What About Eating Fish Instead?
If you’re looking for a safe, proven way to get omega-3s, skip the pills and eat fish. The American Heart Association recommends two 3.5-ounce servings of fatty fish per week. That gives you about 500 mg of EPA and DHA daily-the amount linked to heart benefits in population studies.
Salmon, sardines, mackerel, trout, and anchovies are top choices. They’re rich in omega-3s, protein, and other nutrients like vitamin D and selenium. Plus, you’re not risking oxidation or contamination from low-quality supplements. A 2023 study found people who ate fish twice a week had a 15% lower risk of heart disease compared to those who rarely ate it.
And if you’re vegetarian or vegan? Focus on ALA-rich foods like chia seeds, flaxseeds, hemp seeds, and walnuts. While ALA doesn’t convert well to EPA and DHA, it still has some anti-inflammatory benefits. You might also consider an algae-based DHA supplement-it’s plant-based and doesn’t rely on fish.
The Side Effects and Risks
Fish oil isn’t harmless. At high doses, it can cause:
- Fishy aftertaste or burps (reported by over 30% of users)
- Upset stomach, diarrhea, or nausea
- Bleeding risk-especially if you’re on blood thinners like warfarin or aspirin
- Increased atrial fibrillation (AFib) risk. A 2022 meta-analysis found a 0.4% absolute increase in AFib with high-dose omega-3s. That’s small, but it matters if you’re already at risk for heart rhythm problems.
Also, not all supplements are clean. Some contain mercury, PCBs, or other toxins. Reputable brands test for contaminants and publish results. Look for third-party certifications like USP, NSF, or ConsumerLab. Avoid bargain brands with no testing information.
What Do Doctors Really Think?
There’s a split in the medical community. Dr. Deepak Bhatt, lead researcher of REDUCE-IT, calls high-dose EPA a breakthrough. But Dr. Lee Hooper, who led the 2023 Cochrane review, says the evidence just isn’t there for most people.
A 2024 survey of cardiologists found 68% no longer recommend fish oil supplements for primary prevention. But nearly all still prescribe Vascepa for patients who meet FDA criteria: high triglycerides, existing heart disease, and on statins.
The American Heart Association’s current stance? Don’t use fish oil pills to prevent a first heart attack. But for people with heart failure or those who’ve already had a heart event and still have high triglycerides, it might help. And they still say: get your omega-3s from food first.
The Bottom Line
Fish oil isn’t a magic bullet. It’s not useless, but it’s not for everyone. If you’re healthy, eating fish twice a week is your best bet. If you have high triglycerides, heart disease, or are African American and at risk, talk to your doctor about whether a prescription EPA product like Vascepa could help. Don’t waste money on cheap fish oil pills hoping they’ll save your heart-they probably won’t.
The real takeaway? Your heart doesn’t need a supplement. It needs real food, movement, sleep, and stress management. Fish oil might play a small role for a few people-but it’s not the hero we were sold.
Do fish oil supplements really help your heart?
It depends. For most healthy people, no-standard over-the-counter fish oil supplements don’t reduce heart attacks or death from heart disease. But for people with very high triglycerides, existing heart disease, and who are on statins, high-dose prescription EPA (like Vascepa) has been shown to reduce cardiovascular events by about 25%.
Is EPA better than DHA for heart health?
Evidence suggests EPA alone may be more effective than a mix of EPA and DHA. The REDUCE-IT trial used pure EPA and showed major benefits. The STRENGTH trial used EPA and DHA together and showed no benefit. Researchers think DHA might interfere with EPA’s protective effects, though this isn’t fully proven. No large study has tested pure DHA alone for heart outcomes.
How much fish oil should I take for heart health?
For general heart health, aim for 250-500 mg of EPA and DHA daily from food-not supplements. If you have high triglycerides, your doctor may prescribe 2-4 grams daily of EPA/DHA or pure EPA. Never take high doses without medical supervision, especially if you’re on blood thinners.
Can fish oil lower blood pressure?
Fish oil can slightly lower blood pressure-by about 2-5 mm Hg in people with high blood pressure. But that’s not enough to replace medication. It’s a minor effect, not a treatment. If you’re relying on fish oil to control your blood pressure, you’re not getting the full benefit you need.
Are there better alternatives to fish oil for heart health?
Yes. Eating fatty fish twice a week is more effective than supplements. Other proven strategies include regular exercise, quitting smoking, managing blood pressure and cholesterol with medication if needed, and eating more fiber, nuts, and whole grains. For high triglycerides, statins, fibrates, or prescription omega-3s are more reliable than over-the-counter fish oil.
Is it safe to take fish oil with blood thinners?
High doses of fish oil (over 3 grams daily) can increase bleeding risk, especially when combined with warfarin, aspirin, or other anticoagulants. While standard doses (under 1 gram) are generally safe, always talk to your doctor before combining fish oil with blood thinners. Monitor for signs of unusual bruising or bleeding.
Why did the Cochrane review say fish oil doesn’t work?
The Cochrane review analyzed 79 high-quality randomized trials with over 112,000 people. It focused on the most reliable studies and found that, overall, omega-3 supplements had little to no effect on heart attacks, strokes, or death from heart disease. The studies used standard over-the-counter doses, not the high-dose purified EPA used in REDUCE-IT. So the conclusion applies to most people taking fish oil pills-not those on prescription EPA therapy.
Should I take fish oil if I’m vegetarian or vegan?
If you’re avoiding fish, focus on plant-based ALA sources like flaxseeds, chia seeds, and walnuts. But know that ALA doesn’t convert well to EPA and DHA. For direct EPA and DHA, consider an algae-based supplement. These are vegan, free from ocean contaminants, and provide the same forms of omega-3s your body uses for heart health.


Kevin Narvaes
January 20, 2026 AT 12:17Dee Monroe
January 20, 2026 AT 19:50Ben McKibbin
January 21, 2026 AT 05:16Melanie Pearson
January 22, 2026 AT 10:06Jerry Rodrigues
January 24, 2026 AT 06:04Jarrod Flesch
January 25, 2026 AT 00:53Barbara Mahone
January 26, 2026 AT 05:41Kelly McRainey Moore
January 26, 2026 AT 10:04Samuel Mendoza
January 26, 2026 AT 18:54