Steroid-Adjusted Insulin Calculator
Personalized Insulin Adjustment Tool
This tool helps calculate appropriate insulin adjustments for steroid-induced hyperglycemia. Always consult with your healthcare provider before making changes to your medication regimen.
Recommended Insulin Adjustments
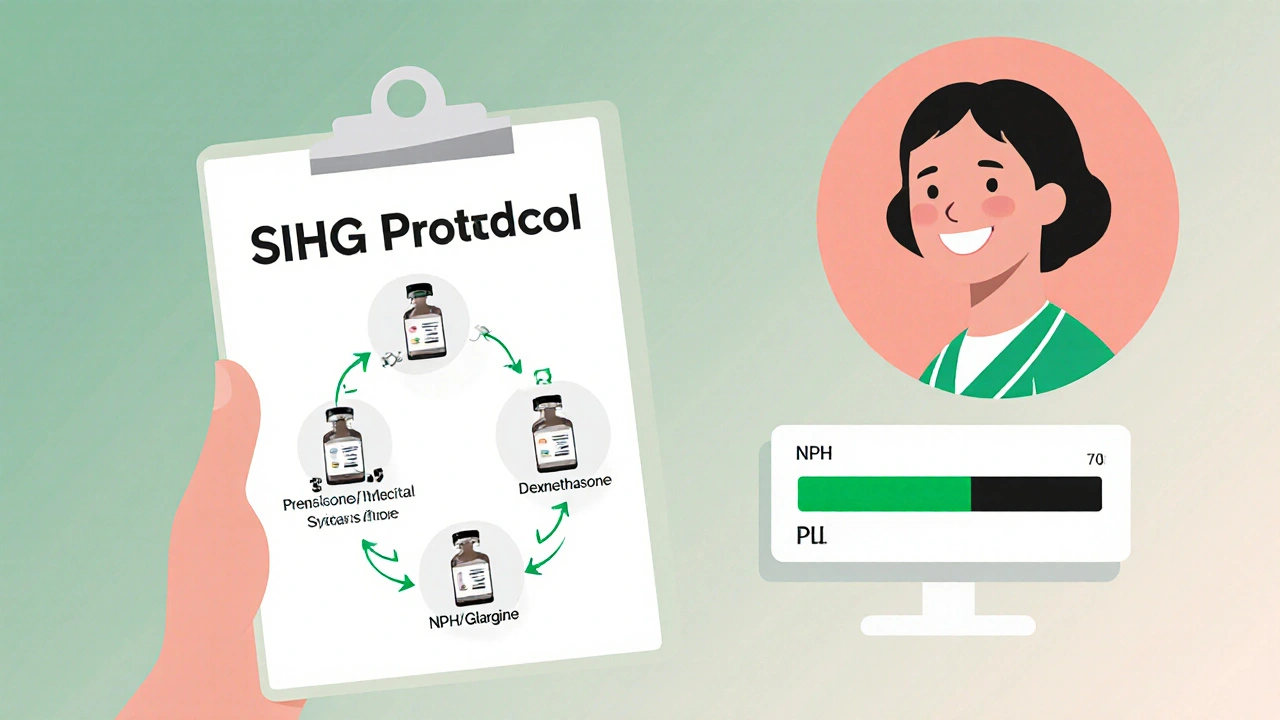
Start insulin adjustment when you begin steroid therapy. For prednisone, use NPH insulin in the morning. For dexamethasone, switch to long-acting analogs like glargine or detemir. Monitor blood sugar every 2-4 hours during peak steroid effect.
When you start taking steroids like prednisone or dexamethasone, your blood sugar can spike-even if you’ve never had diabetes before. This isn’t a fluke. It’s called steroid-induced hyperglycemia, and it happens in 20% to 50% of people on moderate to high doses. For those already living with diabetes, the spike can be even worse. The problem? Most people don’t expect it. And when it hits, they’re left guessing how much extra insulin to take-or worse, they don’t adjust at all.
Why Steroids Raise Blood Sugar
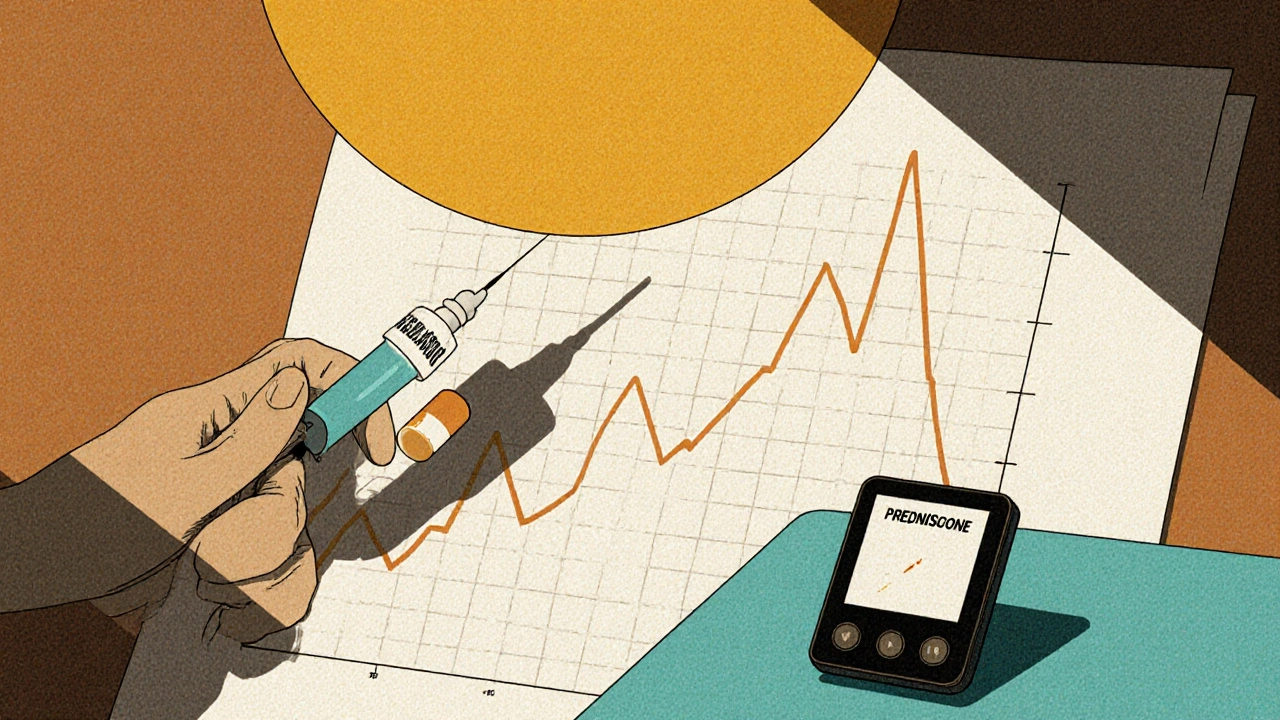
Steroids don’t just reduce inflammation. They also mess with how your body uses insulin. They make your liver pump out more glucose, block insulin from doing its job in muscles and fat, and even dull the signal from your pancreas to release insulin. The result? Blood sugar climbs, often within 4 to 8 hours after taking a steroid dose. It peaks around 24 hours later and can stay high for days after you stop, especially with longer-acting steroids like dexamethasone.Think of it like this: your body is running on a high-sugar setting. Even if you eat the same meals, your blood sugar will climb higher than usual. That’s why simply eating less won’t fix it. You need to adjust your diabetes meds-specifically insulin-to match the steroid’s rhythm.
Insulin Is the First-Line Tool
For most patients, especially those in hospital or on high-dose steroids, insulin is the go-to treatment. Oral medications like metformin or DPP-4 inhibitors might help in mild cases, but they’re not reliable enough when steroid levels are high. Insulin works fast, is predictable, and can be fine-tuned.The standard starting point? Give 0.1 unit of insulin per kilogram of body weight. So if you weigh 70 kg, that’s about 7 units total, split between basal (background) and bolus (meal) insulin. But here’s the catch: timing matters more than the number.
If you’re taking prednisone once a day in the morning, your blood sugar will peak around midday to evening. That means your rapid-acting insulin should be timed to match-not just given at meals. Many people make the mistake of only bolusing for food. But with steroids, you need insulin even if you’re not eating. A correction dose of 0.04 units per kg is recommended if your pre-meal glucose is between 11.1 and 16.7 mmol/L (200-300 mg/dL). If it’s higher than 16.7 mmol/L, use 0.08 units per kg.
Match the Insulin to the Steroid
Not all steroids are the same. And not all insulins work the same way. The key is matching the insulin’s duration to the steroid’s half-life.- Prednisone lasts 18-36 hours. Use NPH insulin in the morning-it peaks around 4-12 hours and lasts up to 18 hours, syncing well with prednisone’s effect.
- Dexamethasone lasts 36-72 hours. Use long-acting analogs like glargine or detemir. NPH won’t last long enough, and you’ll get spikes later in the day.
For example, if you’re on 40 mg of prednisone and normally take 30 units of basal insulin, you might need to add 10-15 units of NPH in the morning. But if you switch to dexamethasone, you’ll need to switch your basal insulin to glargine and increase it by 20-30%.
One real-world tip: if you’ve taken dexamethasone before and needed 20 extra units of insulin, don’t start with 20 again. Start with 10. Titrate up slowly. Steroid effects vary between people-and even between courses.
Monitor Like Your Life Depends on It
You can’t adjust insulin blind. You need data. Capillary blood glucose checks at least four times a day-before meals and at bedtime-are the bare minimum. But if you’re on high-dose steroids or your levels are swinging, check every 2-4 hours.Continuous glucose monitors (CGMs) are game-changers. They show you trends, not just snapshots. The goal? Stay in range-between 3.9 and 10.0 mmol/L (70-180 mg/dL)-at least 70% of the time. And keep time below 3.9 mmol/L under 4%. That’s the new standard from the Joint British Diabetes Societies.
One patient in Brisbane, on a 10-day prednisone course for a flare-up, used her CGM and noticed her glucose jumped at 3 a.m.-even though she hadn’t eaten. That’s the steroid’s delayed effect. She adjusted her basal insulin and avoided a hypoglycemic crash later.
The Biggest Mistake: Not Tapering Insulin with Steroids
Here’s where most people get hurt. When the steroid dose goes down, your blood sugar should drop. But if you keep the same insulin dose? You’re setting yourself up for low blood sugar.Studies show 30-40% of patients on steroids develop dangerous hypoglycemia during tapering because their insulin wasn’t reduced. One man on Reddit shared: “On 40 mg prednisone, I needed 50% more insulin. When I dropped to 20 mg, my doctor didn’t cut my insulin fast enough. I had three hypos in two days.”
That’s why guidelines say: reduce insulin as you reduce steroids. Start cutting insulin 3-4 days after you lower the steroid dose. For every 5 mg drop in prednisone, consider reducing basal insulin by 10-15%. For bolus insulin, cut back as your pre-meal numbers start falling below 10 mmol/L.
And watch out for sulfonylureas. These older diabetes pills force your pancreas to keep releasing insulin-even when your blood sugar is dropping. During steroid tapering, that can cause severe, delayed hypos. A Johns Hopkins study found 27% of patients on sulfonylureas during steroid therapy ended up in the ER for low blood sugar. Switch to insulin if you’re on these drugs.
Special Cases: Type 1 vs. Type 2 Diabetes
Type 1 diabetes patients usually need bigger insulin increases-30-50%-because they have zero insulin production. Type 2 patients often need 20-30% more, depending on how much insulin resistance they already have.Insulin pumps? They’re useful but tricky. You can increase your basal rate by 25-50% during peak steroid effect. But when you taper, you must reduce it just as carefully. A 2022 study found pump users who didn’t adjust their basal rates after steroid reduction had hypoglycemia within 48 hours.
What About Non-Insulin Drugs?
In outpatient settings with mild hyperglycemia (fasting glucose under 11.1 mmol/L), metformin, GLP-1 agonists, or DPP-4 inhibitors can help. But they’re not reliable during hospitalization or with high steroid doses. GLP-1 drugs like semaglutide can be useful for long-term control after steroids end, but they won’t stop the immediate spike.Thiazolidinediones (like pioglitazone) improve insulin sensitivity but take weeks to work. Too slow for steroid-induced spikes. Stick with insulin during active steroid use.
What Hospitals Are Doing Right
Hospitals that use standardized protocols see better outcomes. In 2023, 68% of U.S. hospitals had formal SIHG protocols-up from 42% in 2019. The best ones include:- Automatic insulin dose suggestions based on steroid type and dose
- CGM alerts tied to electronic health records
- Clear guidelines for reducing insulin during tapering
- Education for nurses and doctors on timing
At Massachusetts General Hospital, a quality improvement study found that 37% of errors were caused by not reducing insulin during tapering. Once they added automated alerts in the EHR, those errors dropped by 60%.
Final Takeaway: Anticipate, Match, Reduce
Steroid-induced hyperglycemia isn’t rare. It’s predictable. And it’s manageable-if you act early.Here’s your simple checklist:
- Start insulin before or at the same time as your first steroid dose.
- Match the insulin type to the steroid’s half-life (NPH for prednisone, glargine for dexamethasone).
- Monitor glucose every 2-4 hours during high-dose therapy.
- Use correction doses for high numbers-don’t wait for meals.
- Reduce insulin 3-4 days after lowering your steroid dose.
- Avoid sulfonylureas during steroid therapy.
- Use CGM if you can-it’s the best tool to avoid highs and lows.
Don’t wait for a crisis. Talk to your doctor or diabetes educator before starting steroids. Bring this guide. Ask: “What insulin plan should I start with? When do I reduce it?” Most people don’t ask-and end up in the hospital for something that could’ve been avoided.
Can steroid-induced hyperglycemia turn into type 2 diabetes?
Steroid-induced hyperglycemia doesn’t cause type 2 diabetes, but it can reveal underlying insulin resistance. If your blood sugar stays high after stopping steroids, you may have prediabetes or early type 2 diabetes. A follow-up HbA1c test 3 months after stopping steroids is recommended to check.
How long does steroid-induced high blood sugar last?
It depends on the steroid. Prednisone’s effect fades 3-4 days after the last dose. Dexamethasone can linger for up to a week. Blood sugar usually returns to baseline within 7-10 days after stopping, but insulin doses need to be reduced gradually during that time to avoid lows.
Should I stop taking my diabetes meds if I’m on steroids?
Never stop your meds without medical advice. But you likely need to adjust them. Oral meds like metformin may still be safe, but sulfonylureas should be paused. Insulin usually needs to be increased during steroid use and reduced during tapering. Always work with your healthcare team.
Is it safe to use an insulin pump during steroid therapy?
Yes, but carefully. Increase your basal rate by 25-50% during peak steroid effect. Use temporary basal rates if your pump allows. Monitor closely during tapering-reducing the basal rate too slowly can cause hypoglycemia. Talk to your diabetes team before starting.
What’s the best way to track my blood sugar on steroids?
Use a continuous glucose monitor (CGM) if possible. It shows trends and alerts you to highs and lows. If you don’t have one, check your blood sugar at least four times daily: before meals and at bedtime. More frequent checks (every 2-4 hours) are needed during dose changes or if your sugar is above 16.7 mmol/L.
Can I manage steroid-induced hyperglycemia with diet alone?
No. Diet helps, but steroids override food’s effect on blood sugar. Even a low-carb meal won’t stop a spike caused by prednisone or dexamethasone. Medication adjustment-especially insulin-is necessary. Don’t rely on food changes alone.
If you’re about to start steroids, don’t wait for your blood sugar to climb. Talk to your doctor now. Ask for a personalized insulin plan. Bring this information. You’re not overreacting-you’re being smart.



Shirou Spade
November 25, 2025 AT 06:52Steroids and blood sugar-it’s like your body’s thermostat got hacked by a pharmaceutical glitch. You didn’t ask for this, but now you’re stuck playing whack-a-mole with insulin doses. I’ve seen people crash because they thought, ‘I’ll just eat less.’ Nope. The steroid’s running the show now. You gotta match the drug’s rhythm, not fight it. It’s not about willpower. It’s about pharmacokinetics.
Lisa Odence
November 25, 2025 AT 17:27As a board-certified endocrinologist with over 22 years of clinical experience in metabolic disorders, I must emphasize that the clinical guidelines referenced herein are not only evidence-based but also align with the 2023 American Diabetes Association Standards of Medical Care in Diabetes, which explicitly recommend insulin as the first-line pharmacologic intervention for steroid-induced hyperglycemia, particularly in inpatient settings where glycemic variability is highest and risk of complications-including diabetic ketoacidosis and hyperosmolar hyperglycemic state-is significantly elevated. Moreover, the use of NPH insulin for prednisone and long-acting analogs for dexamethasone is not merely a suggestion-it is a standard of care supported by randomized controlled trials and meta-analyses published in The Lancet Diabetes & Endocrinology and JAMA Internal Medicine. Failure to adhere to these protocols constitutes a deviation from accepted medical practice and may expose clinicians to liability. Please consult your endocrinologist before making any adjustments.
Leisha Haynes
November 27, 2025 AT 11:16lol so you're telling me i need to inject more insulin because some lab-made chemical is telling my liver to throw a sugar party 🤦♀️
guess i'll just keep eating my kale salad and hope for the best
nah jk i'm gonna call my endo tomorrow and make sure they don't forget to taper my insulin like last time when i almost died
seriously though this is wild how no one talks about this until you're in the ER with a glucose of 420
Andrew McAfee
November 29, 2025 AT 06:15Man in India I know was on steroids for asthma and didn't know about the sugar spike. He started feeling dizzy, confused, kept drinking water nonstop. Thought he had the flu. Went to clinic, turned out his sugar was 580. They admitted him. He said he didn't even eat sweets. Just normal rice and dal. Steroids don't care what you eat. They just turn your body into a sugar factory. This needs to be in every doctor's office. Not just for diabetics. For everyone.
Arup Kuri
November 30, 2025 AT 20:56Big Pharma loves this. They sell you the steroid then sell you insulin then sell you CGMs. Meanwhile your pancreas is screaming. They don't want you cured. They want you hooked. Why not just stop the damn steroids? Oh right because they're making billions. And your doctor? They got a free trip to Orlando from Pfizer last year. You think they care about your blood sugar or your paycheck?
They'll tell you to 'manage it' while they cash in. This isn't medicine. It's a business model.
Patricia McElhinney
December 2, 2025 AT 14:10Actually, the recommended correction factor of 0.04 units/kg for BG 200-300 mg/dL is grossly inadequate for most non-obese individuals with type 1 diabetes. The 2022 ISPAD guidelines suggest 0.06-0.10 units/kg for this range, and even higher for those with insulin sensitivity. Furthermore, the statement that 'NPH won't last long enough' for dexamethasone is misleading-glargine U-100 has a duration of 24 hours, but in patients with renal impairment or on high-dose steroids, its pharmacokinetics can be altered, necessitating split dosing or transition to degludec. Additionally, the claim that sulfonylureas cause 27% ER visits is cherry-picked from a single retrospective cohort study with no multivariate adjustment for age, renal function, or concomitant medications. Please cite properly. This post is dangerously oversimplified.
Agastya Shukla
December 2, 2025 AT 18:30From a pharmacodynamic perspective, the glucocorticoid receptor (GR) agonism induces hepatic gluconeogenesis via PEPCK and G6Pase upregulation, while simultaneously downregulating GLUT4 translocation in skeletal muscle-a classic insulin resistance phenotype. The temporal mismatch between steroid half-life and insulin duration is the primary driver of glycemic instability. NPH’s peak action at 4–12 hours aligns with prednisone’s pharmacokinetic profile, whereas dexamethasone’s extended half-life (>36h) requires a flatter, longer-acting basal profile. The correction factor algorithm proposed is clinically sound, but individual titration remains paramount due to inter-individual variability in GR expression and insulin clearance. CGMs are not merely helpful-they are diagnostic tools in this context.
Dolapo Eniola
December 3, 2025 AT 09:49USA doctors always overcomplicate everything. In Nigeria we just give insulin and tell them to eat less rice. Problem solved. Why you need CGM? Why you need 5 different insulins? Just give one shot and move on. Steroids bad, sugar bad, insulin good. Simple. You Americans love your gadgets. We have no money for that. We fix it with common sense and prayer. 😇
giselle kate
December 5, 2025 AT 08:26They say 'antici...pation' but what they really mean is 'corporate greed disguised as medicine'. This whole system is built on keeping you dependent. Why not just ban steroids? Oh right-because they make cancer patients live longer. But guess what? They don't tell you the cost. Your pancreas pays for it. Your kidneys pay for it. Your mental health pays for it. And they charge you for the insulin that fixes what they broke. This isn't science. It's exploitation dressed in white coats.
Shivam Goel
December 5, 2025 AT 10:42Correction: The 0.04 units/kg correction factor is appropriate only for patients with a total daily dose (TDD) of insulin under 0.5 units/kg/day. For those with TDD > 0.6 units/kg/day, the correction factor should be 0.03–0.035 units/kg, per the 2021 ADA Consensus Report on Insulin Dosing. Furthermore, the use of NPH for prednisone assumes a single morning dose; for twice-daily prednisone regimens, split NPH dosing (60/40) or transition to glargine is preferable. Also, the statement that 'dexamethasone lingers for up to a week' is inaccurate-its terminal half-life is 36–72 hours, meaning 94% clearance occurs by day 5. The 7–10 day glucose normalization window reflects residual insulin resistance, not drug persistence. This post contains multiple oversimplifications that could lead to dangerous dosing errors.
Amy Hutchinson
December 6, 2025 AT 19:46i literally just started prednisone yesterday and my sugar was 280 at 2am. i thought i had diabetes. i didn’t even know this was a thing. now i’m scared to sleep. like… what if i die in my sleep? i’m gonna check my sugar every hour. why isn’t this on the pill bottle??
Aki Jones
December 8, 2025 AT 07:58They're lying. This isn't about insulin. It's about the glycemic index of the food they feed you in hospitals. They give you white bread, pasta, and sugary juice-then blame the steroid. The real problem? The system. They want you dependent. They want you buying CGMs. They want you on insulin forever. You think your doctor cares? They get paid per procedure. More insulin = more billing codes. More CGMs = more revenue. You're not sick. You're a product.
Jefriady Dahri
December 9, 2025 AT 07:42Bro this hit different. My mom was on dexamethasone for lupus and we didn’t know anything. She went into ketoacidosis. We thought it was food poisoning. I wish I had this guide then. You’re not just giving info-you’re saving lives. Thank you. I’m printing this out and giving it to every doctor I meet. 🙏💛
Elise Lakey
December 9, 2025 AT 11:10I’m a type 2 on metformin and just started prednisone for a flare. I’ve been checking my sugar every 3 hours. It’s wild how it spikes even after a salad. I’m nervous to start insulin, but this guide makes it feel less scary. I’ll talk to my endo tomorrow. Thank you for writing this so clearly.
Erika Hunt
December 11, 2025 AT 01:03It’s fascinating how a single compound-whether prednisone or dexamethasone-can trigger such a cascade of metabolic dysregulation, disrupting not only glucose homeostasis but also the psychological burden of chronic disease management. The fact that so many patients are unaware of this phenomenon speaks to a systemic failure in patient education, not just in clinical practice but in the way pharmaceutical warnings are communicated. The human cost of this knowledge gap is immense: unnecessary hospitalizations, loss of autonomy, and the erosion of trust in medical advice. Perhaps the most profound takeaway is not the insulin dosing algorithm, but the imperative to treat patients as partners in care-empowering them with information before, not after, the crisis.