When menopause hits, your body doesn’t just stop making estrogen-it changes how your whole system responds to medications you’ve been taking for years. What used to be a harmless pill for anxiety or high blood pressure might now trigger dizziness, nausea, or worse. This isn’t just about hot flashes anymore. It’s about how your body’s new chemistry alters the way drugs work, stick around, or even turn dangerous.
Why Hormone Therapy Changes Everything After Menopause
Your ovaries stop producing estrogen and progesterone. That’s not just a shift in mood or sleep-it’s a full-system reset. And when you start taking hormone replacement therapy (HRT), you’re not just adding back what’s missing. You’re introducing a new variable into a body that’s already adjusting to decades of hormonal change.
The most common HRT options are estrogen-only pills or patches for women who’ve had a hysterectomy, and combination estrogen-progestin for those with an intact uterus. Why the difference? Because estrogen alone can cause the uterine lining to thicken, raising cancer risk. Progestin keeps that lining in check. But adding progestin brings its own side effects: spotting, bloating, breast tenderness. About 30 to 50% of women experience vaginal bleeding in the first six months-most of it stops on its own, but it’s still enough to send people scrambling to their doctors.
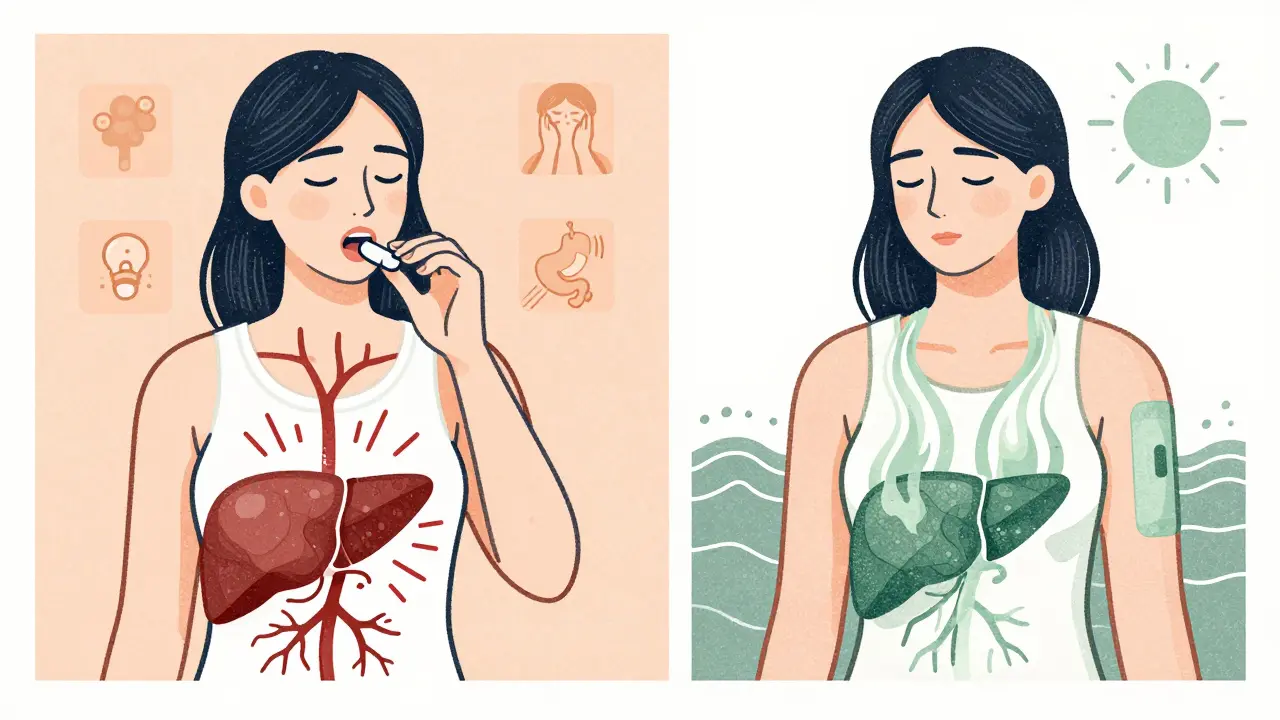
And then there’s the delivery method. Pills are the most common, but they’re also the riskiest. When estrogen goes through your liver, it triggers clotting proteins. That’s why oral HRT increases the risk of blood clots by 2 to 4 times. Patches, gels, and vaginal rings bypass the liver. A 2022 BJOG study found switching from pills to patches cut gastrointestinal side effects by 60%. For women with a history of migraines, liver issues, or clotting disorders, that switch isn’t optional-it’s lifesaving.
The Real Risks You Need to Know
The fear around HRT started with the Women’s Health Initiative study in 2002. It showed that combination therapy increased breast cancer risk by 26%, stroke by 41%, and blood clots by 113%. But here’s what most people miss: those numbers apply mostly to women who started HRT after age 60 or more than 10 years past menopause.
For women who begin therapy before 60 or within 10 years of their last period, the story flips. The North American Menopause Society says the benefit-risk ratio is generally favorable. Your risk of heart disease drops by 30% if you start early. The absolute increase in breast cancer? From 30 cases per 10,000 women to 38 over five years. That’s a small rise-but still real. The FDA warns that hormone therapy may raise dementia risk in women 65 and older by more than double. And gallbladder disease? Risk jumps 77%.
But here’s the truth: you won’t get every side effect. Cancer Research UK puts it bluntly: “Everyone is different.” Some women feel fine on HRT for years. Others get headaches or mood swings after a week. It’s not about avoiding all risk-it’s about matching your personal risk profile to the right treatment.
What Happens When You Take Other Medications?
Menopause doesn’t just change your hormones-it changes how your body processes everything else. A blood pressure pill that worked fine for 15 years might now make you dizzy. An antidepressant might lose its edge. Or worse, it might amplify side effects.
Take Duavee, a combination of conjugated estrogen and bazedoxifene. It’s designed to protect the uterus without needing progestin. But if you’re already on another estrogen or progestin product? That’s a red flag. The FDA’s adverse event database shows 12% of reported problems with Duavee come from mixing it with other hormone meds. Same goes for SSRIs like fluoxetine or paroxetine-they help with hot flashes but can interfere with tamoxifen if you’ve had breast cancer. Gabapentin and clonidine are non-hormonal alternatives that reduce hot flashes by nearly half, but they can cause drowsiness or low blood pressure. Combine those with sleep aids or beta-blockers? You’re asking for trouble.
Even over-the-counter stuff matters. St. John’s wort? It can make HRT less effective. Black cohosh? Studies on 1,845 women show mixed results. Some feel better. Others get liver problems. And don’t assume “natural” means safe.
Non-Hormonal Options That Actually Work
You don’t have to take hormones to feel better. Many women choose alternatives-and they’re not just a backup. They’re often the smarter first move.
For vaginal dryness and painful sex, low-dose DHEA inserts like Intrarosa improve symptoms in 70% of users. Vaginal moisturizers and lubricants? Used by 45% of menopausal women, and they work without systemic effects. For hot flashes, SSRIs reduce them by 50-60% in 60% of users. Gabapentin cuts them by 45%. Clonidine? 46%. These aren’t magic, but they’re real. And they don’t carry the same cancer or clot risks.
Then there’s fezolinetant, a new drug currently under FDA review. In a 2022 trial with 502 women, it slashed moderate-to-severe hot flashes by over 50%-nearly twice as well as placebo. If approved by late 2024, it could become the first non-hormonal, non-antidepressant option approved specifically for menopause symptoms. It targets brain receptors involved in temperature control, not hormones at all.
How to Adjust Your Treatment Without Panic
If side effects hit, don’t quit cold turkey. Talk to your doctor. Most problems can be fixed with small changes.
Here’s what works:
- Lower the dose. Many women get relief on half the standard dose. A 2021 Menopause journal study found 68% of patients improved with dose tweaks.
- Switch delivery methods. Go from pills to patches. It cuts liver strain and GI issues. Patch usage has grown 22% annually since 2018.
- Change the type. Try estradiol instead of conjugated estrogen. It’s a closer match to your body’s natural hormone.
- Use vaginal-only estrogen. If your only symptom is dryness or urinary issues, local estrogen creams or rings give relief with almost no systemic absorption.
And if you miss a dose? Don’t double up. Take it as soon as you remember-but if it’s almost time for the next one, skip it. Double doses can spike hormone levels and trigger spotting or nausea.

Who Should Avoid Hormone Therapy Altogether?
Some women simply shouldn’t take HRT. The American College of Obstetricians and Gynecologists is clear: avoid it if you have:
- A history of breast or endometrial cancer
- Previous stroke or heart attack
- Active blood clots or clotting disorders
- Unexplained vaginal bleeding
- Severe liver disease
And if you’re over 60 and haven’t started HRT? The risks climb fast. The benefit-risk balance tips toward danger. That’s not a rule-it’s a warning.
But if you’re 52, had your last period two years ago, and you’re waking up soaked every night? You’re likely a great candidate. The window is still open. The goal isn’t to live forever-it’s to live well while you can.
What’s Next for Menopause Treatment?
The field is changing fast. New formulations are designed to be safer: lower doses, tissue-specific targeting, non-oral routes. The “window of opportunity” theory-that starting HRT early reduces long-term heart risks-is now mainstream. And the market is responding. The U.S. menopause treatment market hit $1.8 billion in 2022 and is projected to grow 5.3% yearly through 2027.
What’s clear? One-size-fits-all is dead. Your treatment should be as unique as your symptoms, your history, and your goals. It’s not about fear. It’s about smart choices.
Menopause isn’t a disease. It’s a transition. And the right medication can make that transition bearable-even comfortable. But only if you know the risks, the alternatives, and how to adjust as your body keeps changing.
Can hormone therapy cause weight gain during menopause?
Hormone therapy itself doesn’t directly cause weight gain. But the drop in estrogen can slow metabolism and shift fat storage to the abdomen. Many women gain weight around menopause due to aging, reduced activity, and changing hormones-not because of HRT. Some forms of HRT may even help by reducing belly fat in women who start early. If you’re gaining weight, focus on diet, strength training, and sleep-not stopping your meds.
How long should I stay on hormone therapy?
There’s no fixed timeline. Most women take HRT for 2 to 5 years to manage symptoms. But if you’re still having severe hot flashes or bone loss after five years, continuing may be appropriate-especially if you started before 60. The key is regular check-ins with your doctor. Reassess every year. If symptoms fade, try lowering the dose or stopping slowly. Don’t assume you’ll need it forever.
Is it safe to take HRT if I have a family history of breast cancer?
It depends. A family history alone doesn’t automatically rule out HRT. What matters is your personal risk: your genetic profile (like BRCA status), whether you’ve had breast biopsies, and your age. If you have a BRCA mutation or prior breast cancer, HRT is usually not recommended. But if your risk is only slightly elevated and you’re under 60, low-dose, transdermal estrogen might be safer than oral. Talk to a specialist-don’t assume you’re automatically excluded.
Do herbal supplements like black cohosh really help with hot flashes?
Studies on black cohosh are mixed. Twelve trials involving nearly 2,000 women showed no consistent benefit over placebo. Some women swear by it. Others get stomach upset or liver issues. The American College of Obstetricians and Gynecologists warns that most herbal products haven’t been tested for safety or long-term effects. If you try one, stick with reputable brands, avoid high doses, and tell your doctor. Don’t replace proven treatments without a plan.
What should I do if I start bleeding after being postmenopausal for a year?
Call your doctor immediately. Any bleeding after 12 months without a period is not normal, even if you’re on HRT. While spotting in the first 6 months of starting therapy is common, bleeding after that window could signal polyps, endometrial thickening, or even cancer. Your doctor will likely order an ultrasound or biopsy to rule out serious causes. Don’t wait. Don’t assume it’s just the hormones.
Can I switch from pills to patches safely?
Yes, and it’s often a smart move. Patches deliver estrogen through the skin, avoiding the liver and lowering clot risk. Switching can also reduce nausea and bloating. Your doctor can match the dose: for example, a 0.5 mg oral estrogen pill is roughly equal to a 25 mcg patch. You might feel a bit off for a few days as your body adjusts, but most women report fewer side effects within a week.





Alana Koerts
December 19, 2025 AT 11:06Also why is everyone still on oral estrogen? Patches are clearly better.
pascal pantel
December 19, 2025 AT 13:50Gloria Parraz
December 20, 2025 AT 09:45Sahil jassy
December 21, 2025 AT 01:57Kathryn Featherstone
December 22, 2025 AT 19:56Nicole Rutherford
December 23, 2025 AT 17:25Chris Clark
December 25, 2025 AT 06:49Dorine Anthony
December 26, 2025 AT 13:37William Storrs
December 27, 2025 AT 04:22Guillaume VanderEst
December 29, 2025 AT 00:09Dominic Suyo
December 30, 2025 AT 19:06Janelle Moore
January 1, 2026 AT 07:52