More than 10% of Americans carry a label saying they’re allergic to penicillin. But here’s the shocking part: over 95% of them aren’t actually allergic. That label stuck to their medical record from a childhood rash, a stomach ache after a course of antibiotics, or a doctor’s guess decades ago. And it’s costing them more than just inconvenience-it’s putting their health at risk.
Why a False Allergy Label Is a Big Deal
If you’ve been told you’re allergic to penicillin, you’ve probably been given alternatives like vancomycin, clindamycin, or fluoroquinolones. These drugs work, but they’re not better-they’re worse. They’re broader-spectrum, meaning they kill off more good bacteria along with the bad. That’s why patients with fake penicillin allergies are 30% more likely to develop Clostridioides difficile infections, a severe, hard-to-treat gut infection that can land you in the hospital. The CDC estimates that false penicillin allergy labels lead to 50,000 extra cases of this infection every year in the U.S. alone. And it’s not just about infections. These alternative antibiotics are more expensive, often require IV infusions, and increase the risk of antibiotic resistance. Hospitals see patients with fake allergy labels staying longer, needing more tests, and costing nearly $1,000 more per admission. The truth? True penicillin allergies are rare. Only 1-2% of people who think they’re allergic actually have a confirmed IgE-mediated reaction-the kind that causes anaphylaxis. The rest? Their reactions were likely side effects, viral rashes, or just bad timing.How Do You Know If Your Allergy Label Is Real?
You don’t. Not unless you get tested. The old way was to just avoid the drug forever. But modern medicine has a better path: structured allergy testing. It’s not scary. It’s not complicated. And for most people, it’s completely safe. There are two main ways to test:- Skin testing: A tiny drop of penicillin is placed on your skin, then gently pricked. If you’re allergic, a red, itchy bump appears within 15-20 minutes. If that’s negative, a small injection (intradermal) may follow for more certainty.
- Oral challenge: If skin testing is negative, you’re given a small dose of penicillin (like amoxicillin) under observation. After 30-60 minutes, you get a full therapeutic dose. No reaction? You’re not allergic.
What If You Had a Reaction? Does That Mean You’re Allergic?
Not necessarily. Many people think: “I broke out in a rash after amoxicillin-that means I’m allergic.” But rashes are common with viral infections like mononucleosis or even just as a side effect of antibiotics. In fact, up to 20% of all reported penicillin allergies are actually non-allergic side effects-nausea, diarrhea, or a harmless skin rash. True allergic reactions happen fast. Within minutes to an hour. Symptoms include hives, swelling of the face or throat, wheezing, or low blood pressure. If you’ve never had any of those, your risk of a real allergy is extremely low. One patient, a 68-year-old woman with a 40-year-old penicillin label, avoided antibiotics for urinary infections and ended up in the hospital three times. After testing and de-labeling, she was able to take amoxicillin safely. Over two years, she saved over $28,500 in avoidable hospital stays.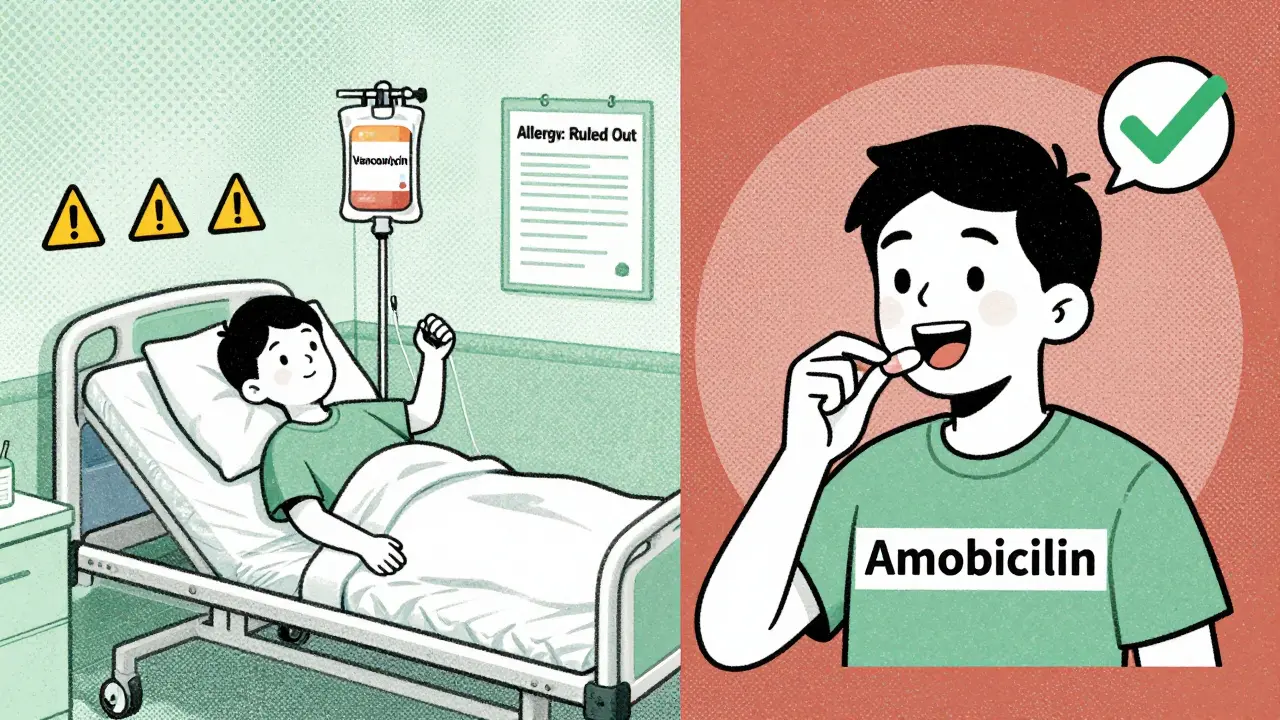
How Testing Is Changing Hospitals (And Why It’s Still Rare)
Some hospitals are leading the way. The University of Pennsylvania’s Penicillin Allergy Relief Program has de-labeled over 1,800 patients since 2020-with zero severe reactions. Epic Systems, the EHR giant used by 84% of U.S. hospitals, now has an automated tool that flags patients with penicillin labels and suggests testing. Since 2021, it’s helped remove nearly 200,000 false labels. The CDC and the Infectious Diseases Society of America now say de-labeling should be part of every hospital’s antibiotic stewardship program. In fact, starting in 2025, Medicare will start rewarding hospitals that reduce inappropriate antibiotic use linked to false allergy labels. So why isn’t everyone doing it? Three big reasons:- Access: There aren’t enough allergists. In rural areas, you might need to drive 200 miles to find one.
- Time: Testing takes an hour or two. Most clinics don’t schedule for it.
- Fear: Patients are scared. Doctors are scared. But the data shows the risk of testing is lower than the risk of avoiding penicillin.
What You Can Do Right Now
If you’ve been told you’re allergic to penicillin:- Ask your doctor: “Was this based on a real allergic reaction, or just a rash or stomach upset?”
- Ask: “Can I be tested to confirm if I’m truly allergic?”
- Ask if your hospital has a penicillin de-labeling program.
- If you’re in a rural area, ask about telemedicine options-some clinics now offer remote evaluations with safe at-home challenges under supervision.
What Happens After You’re Cleared?
Once you pass testing, your allergy label gets removed. Not just “changed”-removed. Your medical record will say “Penicillin allergy: ruled out” or “No penicillin allergy.” That means next time you have an infection, your doctor can prescribe the right drug-amoxicillin, ampicillin, or cefdinir-without needing to reach for stronger, costlier, riskier alternatives. And if you ever need surgery? You’ll be less likely to get a resistant infection. If you’re pregnant? You can safely take penicillin for group B strep, avoiding drugs that might harm your baby. This isn’t just about convenience. It’s about getting the best care possible.What If You Test Positive?
It’s rare-but it happens. If you do have a true allergy, you’ll be given a clear, specific label: “Allergic to amoxicillin,” not “allergic to penicillin.” That’s important. Not all penicillins cross-react. You might still be able to take other beta-lactams safely. You’ll also get an epinephrine auto-injector and instructions on what to do if exposed. And you’ll be advised to wear a medical alert bracelet. Even then, you’re better off knowing the truth. Uncertainty is the real danger.Final Thought: You Deserve the Right Medicine
You wouldn’t take a wrong prescription for your blood pressure. You wouldn’t avoid insulin because someone said you were “sensitive” to it. So why accept a mislabeled drug allergy that’s been holding you back for years? Testing isn’t risky. Not testing is. The science is clear. The tools exist. The hospitals are ready. All you need to do is ask.Can I outgrow a penicillin allergy?
Yes, most people do. Up to 80% of people who had a true penicillin allergy in childhood lose it within 10 years. That’s why anyone labeled allergic as a kid should be retested as an adult-even if they’ve never taken penicillin since.
Is penicillin allergy testing covered by insurance?
Almost always. Most insurance plans, including Medicare and Medicaid, cover skin testing and oral challenges when ordered by a doctor. The cost of testing is typically under $200, compared to the $1,000+ extra cost per hospital stay from using broader antibiotics.
Can I test myself at home?
No. Self-testing is dangerous and not recommended. Even low-risk challenges require medical supervision because reactions, while rare, can happen. But some programs now offer telemedicine consultations followed by supervised at-home challenges with a nurse on video and emergency protocols in place.
What if I had a reaction to another antibiotic like cephalosporin?
Cross-reactivity between penicillin and cephalosporins is much lower than most people think-only about 2% for newer ones. If you reacted to a cephalosporin, you may still be able to take penicillin safely. Testing can clarify this.
How long does the testing process take?
Skin testing takes about 30 minutes. If negative, the oral challenge adds another 1-2 hours of observation. Most people are done in under 3 hours. Some clinics offer same-day results. Others schedule it as a half-day visit.
Will I be able to take penicillin again if I’m cleared?
Yes. Once your label is removed, you can safely take penicillin and related antibiotics like amoxicillin, ampicillin, or cephalexin. You’ll be able to get the most effective treatment for infections without unnecessary risks or costs.





kenneth pillet
January 17, 2026 AT 17:06Been told I’m allergic since I was 8 after a rash. Got tested last year-turned out I’m fine. Took amoxicillin for a sinus infection last month. No drama. Just felt stupid for avoiding it for 30 years.
Kristin Dailey
January 18, 2026 AT 07:55Why are we letting big pharma control our prescriptions? This is just another way they profit off fear.
Naomi Keyes
January 19, 2026 AT 12:16There is a statistically significant discrepancy between self-reported penicillin allergies and confirmed IgE-mediated reactions. The data, as presented, is not only robust but also corroborated by multiple peer-reviewed studies from the CDC and IDSA. Furthermore, the economic burden associated with alternative antibiotic use is quantifiable and alarming.
Praseetha Pn
January 19, 2026 AT 19:59Oh please, they’ve been lying to us for decades. Penicillin is just a gateway drug for the pharmaceutical surveillance state. Once you take it, they track your microbiome, sell your data to insurance companies, and then charge you more for ‘high-risk’ treatments. My cousin in Bangalore got a ‘penicillin alert’ on her medical card after a simple rash-and now her life insurance premiums doubled. They don’t care if you’re allergic-they care if you’re profitable.
And don’t even get me started on how the FDA and WHO are in bed with Big Pharma. That ‘PEN-FAST’ tool? It was designed by a guy who used to work for Pfizer. You think they want you to save money? They want you dependent on their $800 IV antibiotics.
I tested negative, sure-but I still won’t touch penicillin. Not until they open-source the EHR algorithms and let us audit the allergy flags. Until then, I’m sticking with turmeric and garlic. At least those don’t come with a barcode.
Danny Gray
January 20, 2026 AT 23:43So… we’re just supposed to trust a 15-minute skin test over 40 years of bodily intuition? That’s not science. That’s surrender.
What if your immune system remembers? What if it’s just… quiet now? Are we really okay with erasing decades of survival signals for a $200 test? I mean-think about it. Your body knew something. Now they want you to forget.
Jodi Harding
January 21, 2026 AT 03:58I’m 32. Got labeled allergic at 5. Tested at 28. Cleared. Took amoxicillin for strep. Felt like I’d been given back my body. Why did no one tell me this was an option?
Ryan Otto
January 22, 2026 AT 02:04While the data appears superficially compelling, one must interrogate the underlying epistemological framework. The medical establishment’s reliance on IgE-mediated diagnostics as the sole arbiter of ‘truth’ is a reductionist fallacy. Allergy is a systemic phenomenon-not a molecular checkbox. The de-labeling trend is less about patient welfare and more about institutional efficiency. We are medicalizing the body to optimize cost centers, not health outcomes.
Stacey Marsengill
January 22, 2026 AT 21:53My mom died after a reaction to penicillin when I was 10. You think I’m gonna let some doctor poke me with a needle and say ‘you’re fine’? No. I don’t care what your ‘98% accuracy’ says. Some wounds don’t heal with data.
Jake Moore
January 23, 2026 AT 06:39My clinic just started a de-labeling program. We’ve cleared over 120 people since January. Zero reactions. One guy cried because he finally got to eat his grandma’s chicken soup without worrying about antibiotics. This isn’t rocket science. It’s basic care.
Wendy Claughton
January 24, 2026 AT 14:47It’s so beautiful when medicine finally catches up to common sense 💖 I spent 20 years avoiding penicillin because of a rash I got while sick with the flu. Got tested last month. Was cleared. Now I feel like I’ve been given a second chance at health. Thank you for sharing this. 🌿✨
Tyler Myers
January 25, 2026 AT 20:23They say 95% of people aren’t allergic. But what if you’re in the 5% they missed? Who’s gonna pay for your anaphylaxis when they’re too busy cutting costs?
It’s not about fear. It’s about accountability. And nobody’s accountable here.
christian Espinola
January 25, 2026 AT 23:35Incorrect. The term 'allergic' is often misapplied. Side effects ≠ allergies. The CDC data is sound. The medical community is simply correcting a decades-long terminology error. Your ‘allergy’ was never real. Stop romanticizing your ignorance.
Robert Davis
January 26, 2026 AT 09:27They told me I was allergic. I believed them. I avoided penicillin for 40 years. Then I found out my ‘allergy’ was just a rash from a virus. I didn’t need a test. I needed someone to ask me what actually happened. Not just check a box.
Now I’m mad. Not at the medicine. At the system that made me feel like a liability for being sick.