HIV Medication & Birth Control Interaction Checker
Check Your Medication Pairing
This tool shows the interaction risk between your HIV medication and birth control method based on clinical evidence.
Results
When you're living with HIV and taking protease inhibitors to keep your virus under control, your birth control might not be working the way you think it is. This isn't a guess. It's not a myth. It's a documented, well-studied drug interaction that has led to unintended pregnancies in women who took both medications exactly as prescribed.
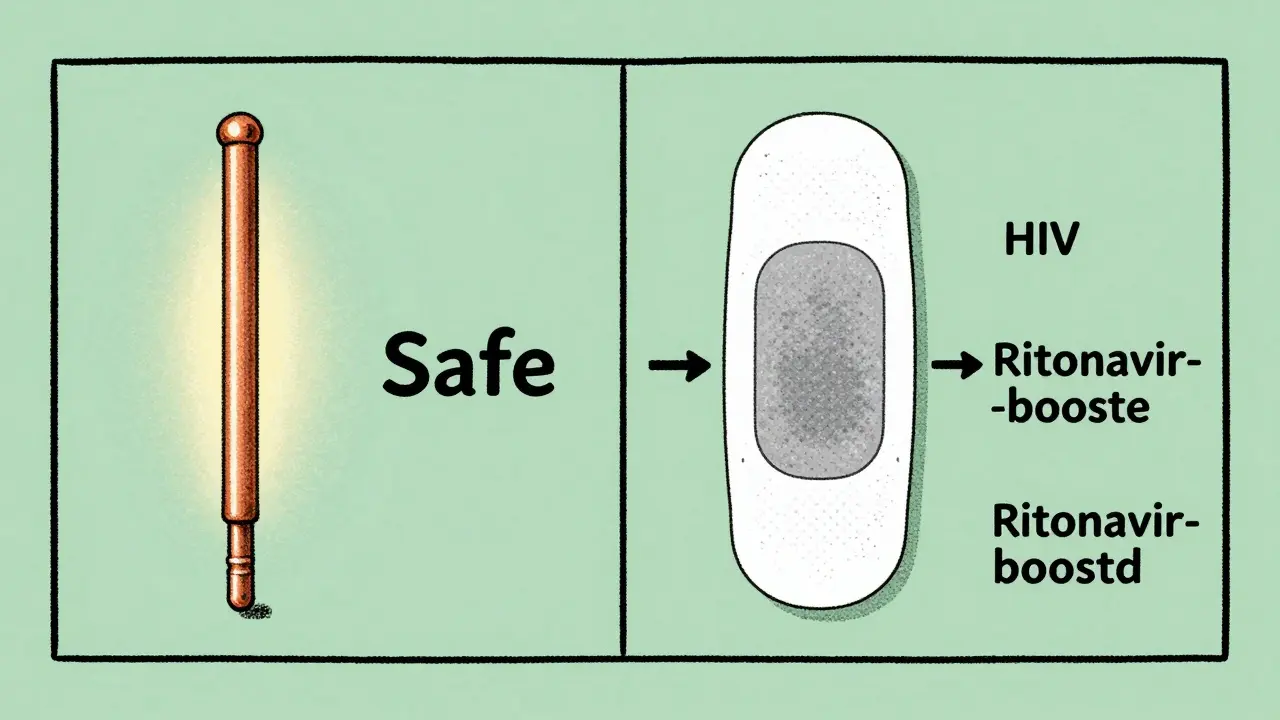
Why This Happens
HIV protease inhibitors - like lopinavir, atazanavir, and darunavir - are often given with a booster called ritonavir to make them work better. But that booster doesn't just help the HIV drug. It messes with your body’s ability to process hormones. These drugs interfere with the CYP3A4 enzyme, which is responsible for breaking down estrogen and progestin in your liver and gut. When this enzyme gets blocked or overstimulated, your contraceptive hormones either drop too low or build up dangerously.For example, in one major study, women using the contraceptive patch while on lopinavir/ritonavir saw their estrogen levels drop by 45%. That’s not a small change. That’s enough to stop ovulation from being suppressed. Another study found that etonogestrel - the hormone in the implant and the vaginal ring - dropped to levels so low that 38% of users were no longer protected. And yet, many women still think, "I’m taking my pill every day, so I’m fine."
Which Birth Control Methods Are Riskiest?
Not all hormonal birth control is affected the same way. Here’s what the data shows:- Combined oral contraceptives (COCs): These are the most vulnerable. Women on efavirenz-based HIV regimens have pregnancy rates as high as 15% - more than double the typical failure rate. Even with perfect use.
- Contraceptive patch and ring: These deliver hormones through the skin or vagina, but they’re still broken down by the same liver enzymes. The ring, in particular, has been shown to fail frequently when used with efavirenz or ritonavir-boosted drugs.
- Progestin-only pills (mini-pills): These are especially risky with ritonavir-boosted regimens. The World Health Organization says they’re a Category 3 match - meaning the risks usually outweigh the benefits. Many women don’t even know this.
- Depo-Provera (injectable): This one’s tricky. Some studies show it’s safe with non-ritonavir drugs, but with efavirenz, pregnancy rates jump to 12.3 per 100 woman-years. That’s higher than most condoms.
- Implants (like Nexplanon): The good news? They’re usually fine with dolutegravir. The bad news? Ritonavir-boosted drugs can slash hormone levels by 40-60%. The International AIDS Society warns against using them together.
And here’s the hard truth: darunavir/cobicistat - a newer, commonly prescribed combo - still reduces levonorgestrel levels by 35%. That’s enough to compromise emergency contraception, too.
What Actually Works?
The only birth control methods that don’t care what HIV meds you’re on are the ones that don’t rely on hormones at all.- Copper IUD: No hormones. No interaction. 99% effective for up to 12 years.
- Hormonal IUD (like Mirena): Even with protease inhibitors, hormone levels stay high enough to prevent pregnancy. Studies show no drop in effectiveness.
- Implants with dolutegravir: New data from 2023 shows this combo is safe. Etonogestrel levels drop only 12% - not enough to matter.
These are called long-acting reversible contraceptives (LARCs). They’re the gold standard for women on HIV treatment. Yet, only 22% of HIV-positive women in low-income countries have access to them. In the U.S., 79% of academic clinics offer them as first-line options. Community clinics? Only 34% do.
Real Stories, Real Consequences
Behind the numbers are real people.One woman on Reddit shared that she got pregnant at 18 weeks while using Depo-Provera and atazanavir/ritonavir. Her doctor told her the interaction was "well-documented but often overlooked." She wasn’t alone. A 2021 survey of 327 HIV-positive women found that 28% had experienced contraceptive failure - and 63% of those were on protease inhibitors.
In another case, a woman in California took Tri-Sprintec daily with darunavir/cobicistat. Her pregnancy test came back positive. She had never missed a pill. Her provider had never warned her about the interaction. She had to choose between stopping her HIV meds - risking viral rebound - or continuing them and accepting the risk of another pregnancy.
Doctors have documented at least 17 such cases in the last decade. And those are just the ones they know about.
What Should You Do?
If you’re on HIV treatment and using hormonal birth control, here’s what you need to do right now:- Check your HIV meds. Are you on a ritonavir-boosted protease inhibitor? That includes lopinavir, atazanavir, darunavir, and nelfinavir. If yes, your birth control might not be working.
- Don’t rely on memory or assumptions. Even if your provider said it was fine five years ago, guidelines have changed. The CDC updated its interaction checker in 2022 with 147 specific drug pairings.
- Ask for a LARC. Say: "I’m on HIV meds. What’s the safest, most effective birth control for me?" Copper IUDs and hormonal IUDs are your best bets.
- Use the CDC’s tool. Go to cdc.gov/hiv/birthcontrol and enter your exact medications. It’s free, fast, and accurate.
And if you’re a provider? Don’t assume your patient knows. Spend seven to ten minutes during every visit talking about this. Use the teach-back method: "Can you tell me in your own words why the pill might not work with your HIV drugs?" Studies show this boosts understanding from 42% to 85%.
The Bigger Picture
This isn’t just about pills and patches. It’s about equity. In sub-Saharan Africa, 63% of clinics can’t insert an IUD on the spot. In the U.S., community health centers are half as likely as academic hospitals to have the right counseling tools. Women in low-income countries are being left behind - not because the science is unclear, but because the systems aren’t built to support them.The good news? The world is moving. Dolutegravir is now the first-line HIV treatment for 72% of new patients. It doesn’t interfere with birth control. That’s huge. By 2030, integrated clinics that offer HIV care and contraception together could cut pregnancy rates among HIV-positive women by two-thirds.
But until then, if you’re on a protease inhibitor, your birth control might be broken. And you deserve to know that.
Can I still use the pill if I’m on HIV protease inhibitors?
No - especially if you’re on ritonavir-boosted drugs like lopinavir/ritonavir or darunavir/cobicistat. Even with perfect use, studies show these combinations can reduce hormone levels enough to cause pregnancy. The WHO classifies this combination as Category 3 - meaning it’s not recommended unless no other options exist.
Is the IUD safe with HIV medications?
Yes. Both copper and hormonal IUDs work just as well whether you’re on protease inhibitors, integrase inhibitors, or any other HIV drug. They don’t rely on liver metabolism, so there’s no interaction. They’re the most reliable choice for women on antiretroviral therapy.
What about the implant (Nexplanon)?
It depends. If you’re on dolutegravir, the implant is safe. But if you’re on ritonavir-boosted protease inhibitors, hormone levels can drop by 40-60%. The International AIDS Society advises against using them together. Always check your specific HIV regimen before choosing an implant.
Does the shot (Depo-Provera) interact with HIV drugs?
It’s complicated. With non-ritonavir drugs like nevirapine, it’s generally safe. But with efavirenz, pregnancy rates jump significantly. Studies show 12.3 pregnancies per 100 woman-years with efavirenz - compared to 5.7 with nevirapine. If you’re on efavirenz, talk to your provider about switching to an IUD.
Why don’t doctors always tell patients about this?
Because many don’t know. A 2018 report found that 41% of women received no counseling about contraceptive interactions when first diagnosed with HIV. Community clinics are far less likely to have training or tools than academic hospitals. The CDC now offers a free 2-hour online course for providers - and over 8,000 have completed it. But awareness is still uneven.
What should I do if I just found out I’m pregnant while on HIV meds?
Don’t panic. Many HIV medications are safe during pregnancy, and continuing treatment reduces the risk of passing HIV to your baby. Talk to your provider immediately about your HIV regimen and pregnancy. Do not stop your HIV meds on your own. You can still have a healthy pregnancy with the right care.





Siobhan K.
December 21, 2025 AT 03:51Brian Furnell
December 23, 2025 AT 02:56Ben Warren
December 23, 2025 AT 12:01Sandy Crux
December 23, 2025 AT 12:35Hannah Taylor
December 23, 2025 AT 15:43Jay lawch
December 25, 2025 AT 09:51Dan Adkins
December 27, 2025 AT 08:21Grace Rehman
December 29, 2025 AT 05:44Adrian Thompson
December 29, 2025 AT 16:32John Hay
December 31, 2025 AT 06:29Jon Paramore
December 31, 2025 AT 20:46Swapneel Mehta
January 1, 2026 AT 17:06Stacey Smith
January 3, 2026 AT 08:00Jason Silva
January 3, 2026 AT 16:08mukesh matav
January 4, 2026 AT 12:22