Anticoagulant Suitability Calculator
Find the best blood thinner for your health profile
Answer these questions to see which anticoagulant is safest for you based on current medical guidelines. Your personal health condition is the most important factor in this decision.
When you need a blood thinner, the choice between DOACs and warfarin isn’t just about which pill to take-it’s about how that choice affects your daily life, your risk of bleeding, and your long-term health. For millions of people with atrial fibrillation or a history of blood clots, this decision matters more than most realize. And the data since 2020 has made one thing clear: DOACs are now the go-to for most patients. But that doesn’t mean warfarin is obsolete. Each has its own risks, and knowing the difference could literally save your life.
How DOACs and Warfarin Work Differently
Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting factors. That sounds simple, but your diet, other medications, and even your genes can throw it off. One day your INR (a blood test that measures clotting time) might be perfect. The next, after eating a big salad, it drops. That’s why people on warfarin often need weekly blood tests.
DOACs-like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa)-work differently. They directly block specific proteins in the clotting process: either factor Xa or thrombin. You don’t need to watch your spinach intake. You don’t need weekly blood tests. You take a fixed dose, once or twice a day, and it just works.
This isn’t just convenient. It’s safer. Studies show DOACs reduce the risk of dangerous bleeding by about 30% compared to warfarin. That’s not a small difference. It’s the reason doctors now prescribe DOACs for 75% of new patients.
Bleeding Risks: What the Numbers Really Show
All blood thinners increase bleeding risk. But not all bleeding is the same. The biggest concern with warfarin is intracranial hemorrhage-bleeding in the brain. That’s often fatal. DOACs cut that risk by 50-60%. That’s huge. In a 2023 study of nearly 18,500 patients with blood clots, those on DOACs were 31% less likely to be hospitalized for major bleeding than those on warfarin.
But not all DOACs are equal. Apixaban has the lowest bleeding rate among them-just 1.9 events per 100 person-years. Rivaroxaban is higher, at 2.8. Warfarin sits at 2.4. So if you’re choosing a DOAC, apixaban is the safest bet for most people, especially if you’re over 75 or have kidney issues.
There’s another twist: gastrointestinal bleeding. DOACs like rivaroxaban carry a higher risk here than apixaban. If you’ve had stomach ulcers or GI bleeding before, your doctor might avoid rivaroxaban entirely.
When Warfarin Is Still the Better Choice
DOACs aren’t perfect for everyone. If you have a mechanical heart valve-like a metal one implanted after heart surgery-DOACs are dangerous. They can cause clots to form on the valve, leading to stroke or heart attack. Warfarin is the only approved option here.
Same goes for antiphospholipid syndrome. This rare autoimmune condition makes your blood extra prone to clotting. Studies show DOACs are 2.8 times more likely to cause clots in these patients than warfarin. That’s why rheumatologists still recommend warfarin for this group.
And if your kidneys are severely damaged-CrCl under 15-30 mL/min-some DOACs can’t be used safely. Apixaban and edoxaban can still be used at lower doses, but dabigatran is off the table. Warfarin doesn’t rely on kidney function, so it’s often the only option left.
Monitoring, Diet, and Drug Interactions
Warfarin has over 1,000 known drug interactions. Antibiotics, painkillers, even herbal supplements like St. John’s wort can change how it works. And vitamin K in foods like kale, broccoli, and spinach can make it less effective. One patient on PatientsLikeMe reported her INR dropped from 2.5 to 1.8 in just 48 hours after eating a large spinach salad-even though she took her dose the same.
DOACs? About 50-100 interactions max. No diet restrictions. No weekly blood tests. That’s why 89% of DOAC users say they feel more freedom in their daily lives. And 85% say they’re less stressed about forgetting to get lab work done.
But here’s the catch: if you miss a dose of a DOAC, especially rivaroxaban or dabigatran, your protection drops fast. Their half-lives are only 5-17 hours. Warfarin lasts 20-60 hours. So missing one dose of warfarin isn’t as risky as missing one of a DOAC.
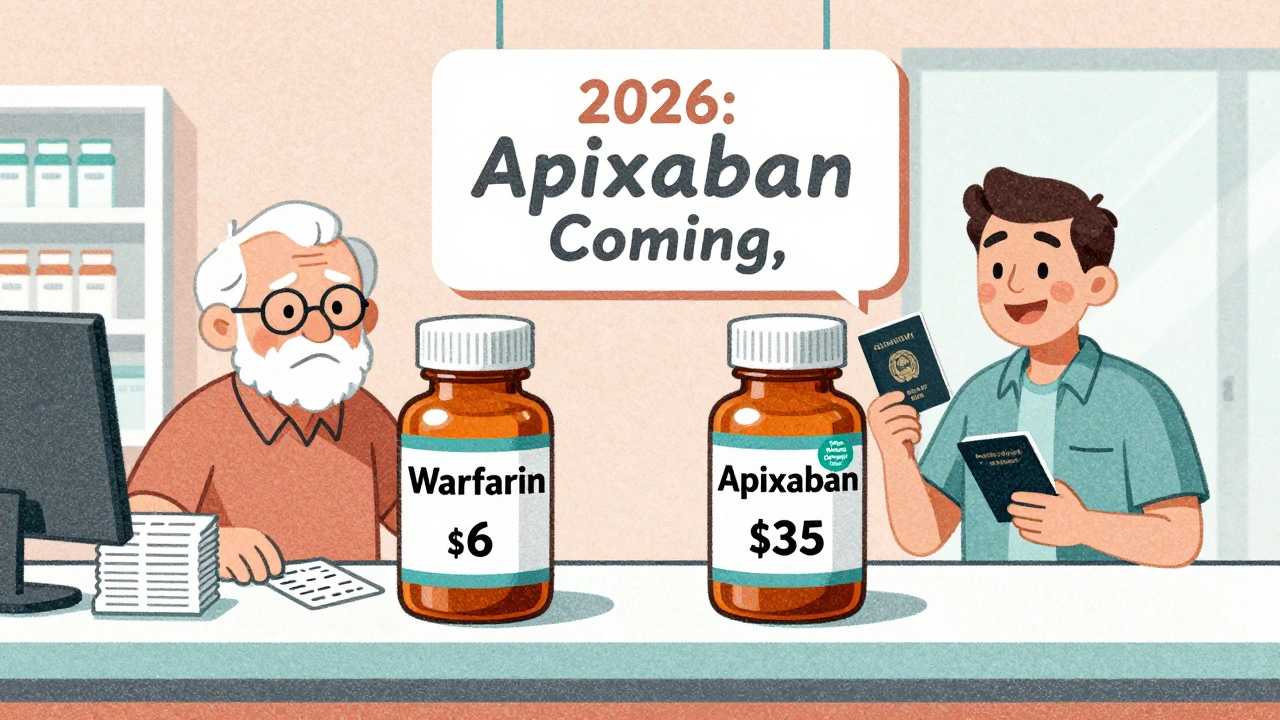
Cost: The Hidden Barrier
Warfarin costs $4 to $10 a month. DOACs? $450 to $600 without insurance. That’s a huge gap. But most people don’t pay full price. Medicare Part D and private insurers cover DOACs, usually with a $30-$100 copay. Still, for those on fixed incomes or without good coverage, warfarin is the only affordable option.
And here’s something most don’t realize: warfarin isn’t cheap when you add in the cost of monitoring. If you get 13 or more INR tests a year, the total cost of warfarin-including blood tests, doctor visits, and time off work-equals or exceeds that of a DOAC. That’s why insurers now favor DOACs. They’re not just safer-they’re more cost-effective in the long run.
Real-Life Patient Experiences
On Reddit’s r/bloodthinners, a common complaint is the emotional toll of warfarin. One user wrote: “I felt like a lab rat. Every week, I’d panic before my INR came back. If it was too high, I’d be on bed rest. Too low, and I’d be scared to walk the dog.”
Another said: “I switched to apixaban and didn’t realize how much anxiety I was carrying until it was gone. I travel now. I eat what I want. I don’t check my calendar for blood test days.”
But cost still bites. A 2023 survey found 63% of DOAC users worried about affordability. Some skip doses. Others go without refills. That’s dangerous. A 2022 CVS Health analysis showed 28% of warfarin users quit within a year-mostly because of the hassle. Only 18% of DOAC users did. The burden of monitoring is a real reason people stop taking their meds.
Who Gets Which Drug? A Quick Guide
Doctors now use simple tools to pick the right one. If you’re over 80, have kidney issues, or have had bleeding before, apixaban is usually the best DOAC. If you’re younger, healthy, and have no GI history, any DOAC works. If you have a mechanical valve, antiphospholipid syndrome, or very poor kidney function-stick with warfarin.
And don’t forget: your doctor should check your kidney function every 6-12 months if you’re on a DOAC. Dosing errors happen in nearly 1 in 5 cases. Too much DOAC in someone with kidney problems? Higher bleeding risk. Too little? Higher stroke risk.
What’s Next? Reversal Agents and New Options
If you bleed badly on warfarin, doctors can give you vitamin K or a concentrated clotting factor. It works, but it takes hours.
For DOACs, we have specific antidotes now. Idarucizumab reverses dabigatran in minutes. Andexanet alfa reverses apixaban and rivaroxaban. These aren’t perfect-they’re expensive and not always available-but they’re game-changers in emergencies.
Even better? Two new reversal agents are in late-stage trials. One works on all anticoagulants. That could mean fewer deaths from bleeding, no matter which drug you’re on.
By 2026, generic apixaban will hit the market. Rivaroxaban will follow in 2027. That could cut DOAC costs by 70-80%. When that happens, the choice won’t just be about safety-it’ll be about access.
Bottom Line: What You Need to Know
For most people-especially those with atrial fibrillation or a blood clot-DOACs are the better choice. They’re safer, simpler, and more predictable. Apixaban has the best safety record among them.
But if you have a mechanical heart valve, antiphospholipid syndrome, or severe kidney disease, warfarin is still your best option. And if cost is a barrier, talk to your doctor about patient assistance programs. Many manufacturers offer free or low-cost DOACs for those who qualify.
Don’t let fear of side effects keep you from taking your medicine. The real danger isn’t the drug-it’s not taking it at all. The key is picking the right one for you, and sticking with it.
Are DOACs safer than warfarin?
Yes, for most people. DOACs reduce the risk of major bleeding by about 30% compared to warfarin, especially dangerous brain bleeds. Apixaban has the lowest bleeding risk among DOACs. But safety depends on your health-DOACs aren’t safe for everyone, like those with mechanical heart valves.
Can I switch from warfarin to a DOAC?
Most people can, but it’s not automatic. Your doctor will check your kidney function, bleeding history, and whether you have conditions like antiphospholipid syndrome or a mechanical valve. If you’re eligible, switching improves safety and convenience. Never switch on your own-timing matters to avoid clotting or bleeding risks.
Do I need blood tests with DOACs?
No routine blood tests are needed for DOACs. But your doctor should check your kidney function every 6-12 months, especially if you’re older or have other health issues. Dosing depends on kidney health, and skipping these tests can lead to dangerous under- or overdosing.
What’s the cheapest blood thinner?
Warfarin is the cheapest-$4 to $10 a month. DOACs cost $450-$600 without insurance, but most people pay $30-$100 with coverage. If you’re struggling with cost, ask about manufacturer assistance programs. Some DOAC makers offer free medication to those who qualify.
Can I drink alcohol on DOACs or warfarin?
Moderate alcohol is usually okay with both, but heavy drinking increases bleeding risk with either drug. With warfarin, alcohol can also make your INR unpredictable. If you drink regularly, tell your doctor. They may recommend avoiding alcohol or switching to a DOAC for more stable control.
What happens if I miss a dose of a DOAC?
If you miss a dose of apixaban or edoxaban, take it as soon as you remember-but only if it’s within 6 hours. If it’s been longer, skip it and take your next dose on time. For rivaroxaban or dabigatran, take it within 12 hours; otherwise, skip it. Never double up. Missing doses increases stroke risk, especially with DOACs because they leave your system faster than warfarin.





Nigel ntini
December 5, 2025 AT 16:22DOACs changed my life. No more weekly finger pricks, no more worrying about spinach. I travel internationally now without panic. Apixaban’s the one. Simple, reliable, and I actually remember to take it.
Priya Ranjan
December 5, 2025 AT 19:56People don’t realize how dangerous these new drugs are. No monitoring? No oversight? This is pharmaceutical greed disguised as innovation. Warfarin has 70 years of data. These DOACs? Half-baked science with a marketing budget.
Gwyneth Agnes
December 6, 2025 AT 13:24Apixaban beats warfarin. Period.
Ashish Vazirani
December 7, 2025 AT 23:53Who the hell is giving this advice? In India, we don’t even have access to these fancy pills. They’re for rich Americans who can afford $600/month. Meanwhile, we’re stuck with warfarin-and we manage just fine. Why are you pushing this Western bias? We don’t need your ‘convenience’-we need affordability!
Mansi Bansal
December 9, 2025 AT 17:19One must acknowledge the profound epistemological implications of anticoagulant selection. The ontological shift from vitamin K antagonism to direct thrombin inhibition represents not merely a pharmacological evolution, but a sociopolitical reconfiguration of patient autonomy vis-à-vis institutional medical authority. The commodification of therapeutic simplicity, while ostensibly liberating, paradoxically engenders a latent vulnerability through pharmacokinetic fragility-particularly in populations lacking robust healthcare infrastructure. One cannot, therefore, reduce this decision to a binary of efficacy versus cost; it is, rather, a moral calculus embedded within the architecture of global health inequity.
Kay Jolie
December 10, 2025 AT 16:21Okay but have you considered the pharmacoeconomic ripple effect? DOACs aren’t just ‘safer’-they’re disruptors in the care delivery ecosystem. Reduced INR visits mean fewer clinic touchpoints, which shifts burden to primary care, which reduces specialist overload-BUT-only if you have insurance that doesn’t nickel-and-dime you. Also, the reversal agents? Pure sci-fi magic. Idarucizumab is like a medical deus ex machina. I’m just saying… we’re living in the future, y’all.
pallavi khushwani
December 11, 2025 AT 12:34I used to be terrified of blood thinners. Warfarin made me feel like my body was a broken machine. Switching to apixaban didn’t just change my meds-it changed how I felt about myself. I stopped checking my INR like a prayer. I started going for walks again. Sometimes the simplest things-like not having to plan your life around a lab appointment-are the most revolutionary.
Billy Schimmel
December 12, 2025 AT 16:20So you’re telling me the drug that costs $4 a month is the ‘bad’ one because it needs blood tests… and the one that costs $600 is the ‘good’ one because it’s ‘convenient’? Wow. What a world. I bet your dog takes DOACs too.
Shayne Smith
December 13, 2025 AT 16:56My grandma’s on warfarin. She’s 84. Loves her weekly blood test. Says it’s her ‘appointment with the universe.’ I don’t get it, but I respect it. She’s alive and happy. Maybe the real answer isn’t which drug is better… but which one lets you live your life.
Geraldine Trainer-Cooper
December 15, 2025 AT 16:35DOACs are just another way capitalism makes you pay for peace of mind. You don’t need a blood test. You need a revolution. The real side effect? Being made to feel guilty for not being able to afford your safety.
Nava Jothy
December 16, 2025 AT 19:33Apixaban? 😍 I take it with my morning matcha and yoga. Warfarin? 🤮 I used to have nightmares about spinach. Now I eat kale like a goddess. Also, my nails are stronger. Coincidence? I think not. #DOACGlowUp
Kenny Pakade
December 18, 2025 AT 14:53DOACs were created by Big Pharma to replace warfarin because they realized Americans are too lazy to get blood tests. It’s all a scam. The real reason they’re pushing DOACs? So you’ll die quietly from a brain bleed and they won’t have to pay for your ICU. Also, why is there no long-term data? Where’s the 20-year study? Hmm?
brenda olvera
December 19, 2025 AT 14:10My cousin in Lagos is on warfarin. He walks 10km to the clinic every week. He doesn’t complain. He just takes his pill. Sometimes I think we in the US forget what real healthcare looks like. Not every solution needs to be high-tech. Sometimes it’s just someone showing up.
Myles White
December 21, 2025 AT 07:32Let’s not forget the flip side. DOACs are great for people with good kidneys, good insurance, and good memory. But what about the elderly with dementia? Or the homeless? Or the ones who can’t afford to miss work for a 15-minute kidney check? I’ve seen patients on DOACs who didn’t know their own dosage. One guy took three pills because he thought ‘twice daily’ meant ‘three times.’ He bled internally. Took three days to diagnose. Warfarin’s hassle? At least you’re being watched. DOACs? You’re on your own. And that’s terrifying.
It’s not about which drug is better. It’s about whether the system supports you taking it safely. And right now? It doesn’t.
olive ashley
December 21, 2025 AT 19:17They’re hiding something. Why are reversal agents so expensive? Why are DOACs banned in some countries? Why do the trials always exclude people over 85? I’ve got a friend who had a stroke on apixaban. The doctor said ‘it’s rare.’ But it happened to her. And now she’s in a nursing home. You think this is science? It’s a gamble. And you’re the one holding the dice.