When your sodium levels drop too low, it’s not just a lab result-it’s fatigue, confusion, nausea, and sometimes seizures. Hyponatremia doesn’t always respond to salt pills or fluid restriction. For many, Natrise (tolvaptan) becomes the next step. But it’s not the only option. And it’s not always the best one. If you’re weighing Natrise against other treatments, you’re not alone. Doctors see this choice every day. Patients ask: Is there something safer? Cheaper? More effective? Let’s break down what’s actually out there.
What Natrise (Tolvaptan) Actually Does
Natrise is a vasopressin receptor antagonist. That’s a fancy way of saying it blocks the hormone that tells your kidneys to hold onto water. When you have SIADH (syndrome of inappropriate antidiuretic hormone secretion), your body keeps reabsorbing water even when it shouldn’t. That dilutes your blood sodium. Natrise forces your kidneys to flush out excess water-without losing sodium. It’s a water diuretic, not a salt diuretic.
It’s approved for euvolemic and hypervolemic hyponatremia, especially when caused by SIADH or heart failure. The standard dose is 15 mg once daily, with a max of 60 mg. You’ll see urine output increase within hours. Sodium levels usually rise by 4-6 mmol/L in the first day. But here’s the catch: it can raise sodium too fast. That’s dangerous. Too quick a correction can cause osmotic demyelination syndrome-a rare but devastating brain injury.
The FDA warns that Natrise should only be started in a hospital setting for the first dose. Outpatient use requires strict monitoring. And it’s expensive. In Australia, a 30-day supply can cost over $800 without subsidy. That’s why many look at alternatives.
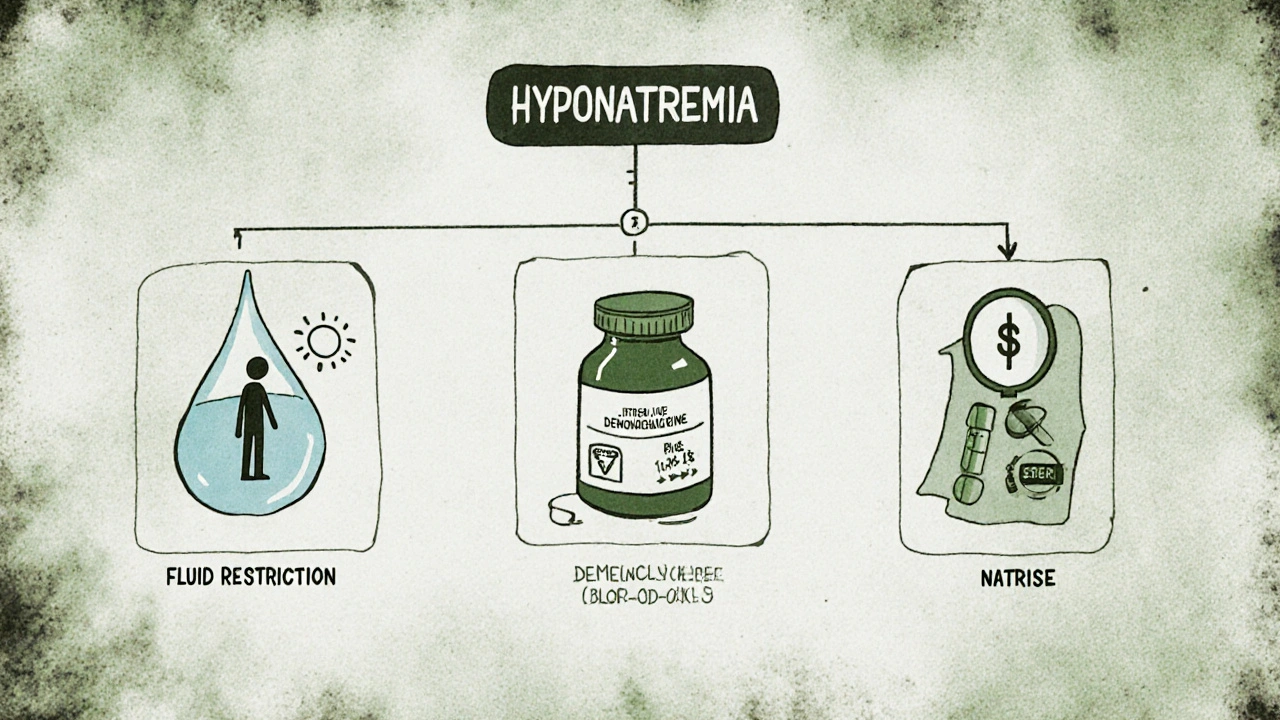
Fluid Restriction: The Old-School Approach
Before drugs like Natrise, doctors told patients to drink less. Like, a lot less. Often under 1 liter per day. For some, especially those with mild SIADH from medications or lung cancer, this works. It’s free. No side effects. No prescriptions.
But it’s hard. Really hard. Thirst is a powerful drive. People get headaches, dry mouth, irritability. Compliance drops fast. One 2023 study in the Journal of Clinical Endocrinology & Metabolism found that only 38% of patients stuck with fluid restriction for more than 3 months. And if sodium doesn’t improve in 48 hours, you’re back to square one.
Fluid restriction works best as a first step-or as a maintenance plan after Natrise has done its job. It’s not a replacement for drug therapy in moderate to severe cases. But it’s still a tool. And it’s the only one that doesn’t cost a dime.
Demeclocycline: The Antibiotic That Helps Your Sodium
Demeclocycline is a tetracycline antibiotic. But it’s not used for infections here. It’s used because it causes nephrogenic diabetes insipidus-meaning it makes your kidneys ignore vasopressin. Sound familiar? That’s exactly what Natrise does. Only demeclocycline does it by damaging the kidney’s ability to concentrate urine.
It’s cheaper. A 30-day supply costs under $50 in Australia. It’s taken orally, twice daily. Effects show up in 3-5 days. Sodium levels rise slowly and steadily. That’s a plus. Slower correction means lower risk of brain damage.
But the trade-offs are real. It can cause sun sensitivity, nausea, and yeast infections. Long-term use risks kidney damage. It’s also not approved for hyponatremia in Australia-so it’s off-label. Not every doctor will prescribe it. And if you’re over 65 or have liver disease, it’s usually avoided.
Still, for patients who can’t afford Natrise or need long-term management, demeclocycline is a real option. It’s not perfect. But it’s been used for decades. And it works.
Conivaptan: The IV Alternative
Conivaptan is the injectable cousin of tolvaptan. It’s given intravenously in hospitals. It blocks both V1a and V2 vasopressin receptors. That means it not only helps with water excretion but also causes mild vasoconstriction. That’s useful if you’re in the ICU with heart failure and low sodium.
It works fast. Sodium levels can rise within 24 hours. It’s approved for hospitalized patients with euvolemic or hypervolemic hyponatremia. But it’s not for home use. You need IV access, constant monitoring, and a critical care team.
Compared to Natrise, conivaptan is more aggressive. It’s used when you need a quick correction-like in someone with seizures or altered mental status. But once stabilized, you’re usually switched to oral therapy. Natrise is the natural next step.
Conivaptan’s biggest downside? Cost. And access. It’s not stocked in most community hospitals. If you need it, you’re likely in a major city hospital. It’s a bridge-not a long-term solution.
Other Options: Urea, Salt Tablets, and More
Urea is an old-school osmotic agent. It’s not a drug in most countries, but it’s available as a powder. You mix it in water and drink it. It draws water out of your blood by increasing osmotic pressure. In a 2022 trial in the European Journal of Internal Medicine, urea raised sodium levels as well as tolvaptan in SIADH patients-with fewer side effects.
It’s cheap. A month’s supply costs less than $30. It tastes awful-like bitter chalk-but many patients get used to it. It’s especially useful in elderly patients or those with kidney disease, where water restriction is risky.
Salt tablets? They’re tempting. But they rarely work alone. Your body just pees out the extra sodium if vasopressin is still active. They’re usually combined with other treatments-not standalone.
Loop diuretics like furosemide? They help in heart failure patients by reducing fluid overload. But they also wash out sodium. They’re not for SIADH. Misuse can make hyponatremia worse.
Which Option Is Right for You?
There’s no one-size-fits-all. Here’s how real patients and doctors decide:
- Acute, severe hyponatremia (sodium <120 mmol/L, confusion, seizures) → Hospital IV treatment with conivaptan or hypertonic saline, then transition to oral therapy.
- Chronic SIADH, young and healthy, can afford it → Natrise. Fast, effective, well-studied.
- Chronic SIADH, elderly, on a budget, or kidney issues → Urea or demeclocycline. Slower but safer long-term.
- Mild cases, no symptoms, no comorbidities → Fluid restriction first. Recheck in 2 weeks.
- Heart failure with hyponatremia → Furosemide + fluid restriction + possibly Natrise if other options fail.
One thing all doctors agree on: sodium correction must be gradual. Never raise sodium by more than 8-10 mmol/L in 24 hours. That’s non-negotiable. Even with Natrise, you need daily blood tests for the first week.
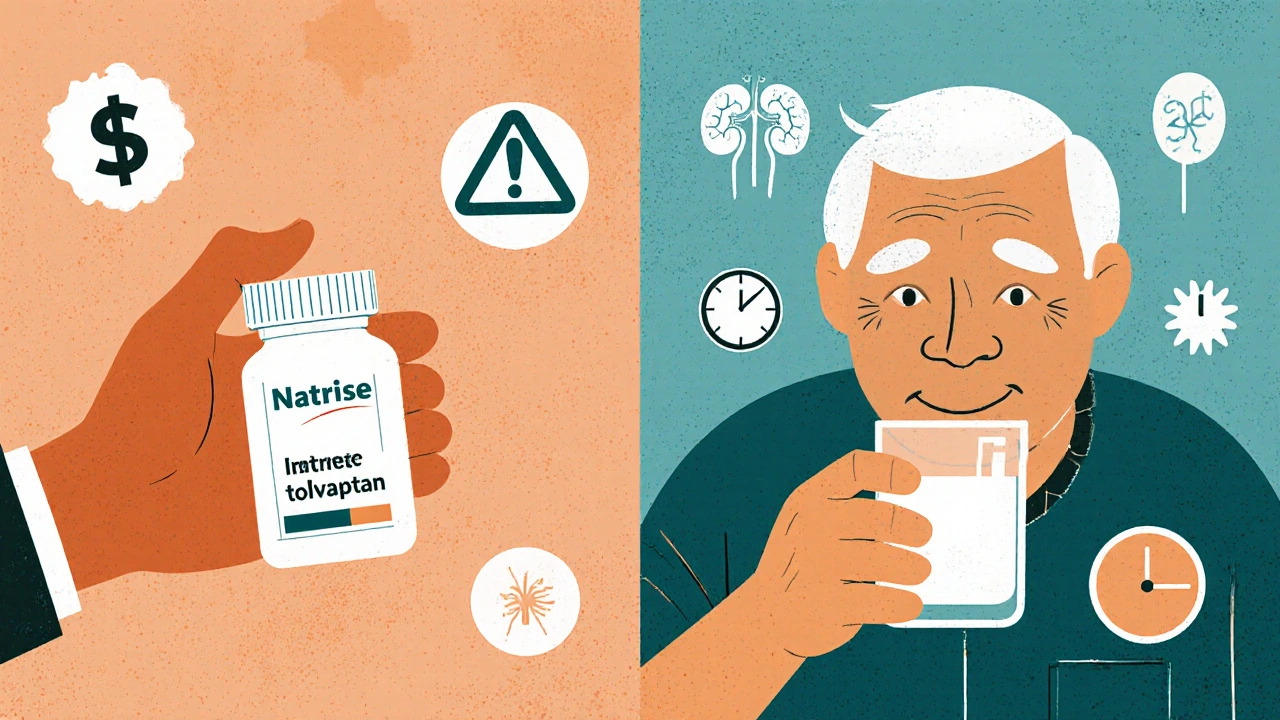
The Real Cost of Natrise
In Australia, Natrise isn’t on the PBS (Pharmaceutical Benefits Scheme) for SIADH. That means full price. $800-$1,200 per month. Demeclocycline? $45. Urea? $25. Conivaptan? $2,000+ per hospital stay.
Insurance won’t cover Natrise unless you’ve tried everything else. Many patients get denied. That’s why off-label options matter. Doctors don’t always tell you about cheaper alternatives because they’re not marketed. But they’re used.
If you’re paying out of pocket, ask your doctor about urea. It’s not glamorous. But it’s effective. And it doesn’t require weekly blood tests like Natrise.
What Happens If Nothing Works?
Some patients don’t respond to any of these. That’s when you dig deeper. Is it really SIADH? Could it be adrenal insufficiency? Hypothyroidism? Medication side effect? Sometimes, stopping a drug like SSRIs or carbamazepine fixes everything.
And if you’ve tried all the drugs? You might need a specialist. Endocrinologists and nephrologists see these cases regularly. They know the latest trials. They might suggest clinical trials for new drugs like lixivaptan or satavaptan-still experimental, but promising.
Don’t give up. Hyponatremia is treatable. But it takes patience. And the right match between drug and patient.
Is Natrise better than demeclocycline?
Natrise works faster and is more predictable, but it’s expensive and requires close monitoring. Demeclocycline is cheaper and safer for long-term use, but it takes days to work and can cause side effects like sun sensitivity and kidney stress. For most people needing quick results, Natrise wins. For long-term management, especially on a budget, demeclocycline is often preferred.
Can I take Natrise at home?
Yes-but only after your first dose is given in a hospital. Your doctor needs to confirm your sodium levels are rising safely before you take it at home. You’ll need weekly blood tests for the first month. If your sodium jumps too fast, you’ll need to stop immediately.
Why isn’t Natrise covered by Medicare in Australia?
Natrise isn’t listed on the PBS for SIADH because the government considers it too expensive compared to alternatives like fluid restriction or demeclocycline. It’s only covered for autosomal dominant polycystic kidney disease (ADPKD), not hyponatremia. That means most patients pay full price unless they qualify for a special access scheme.
Does urea really work as well as Natrise?
Yes-in multiple studies. A 2022 trial showed urea raised sodium levels just as effectively as tolvaptan in SIADH patients, with fewer side effects. The main drawback is taste and compliance. Some patients can’t stand the flavor, but many adapt. It’s a solid, low-cost alternative.
What are the risks of correcting sodium too quickly?
Raising sodium by more than 8-10 mmol/L in 24 hours can cause osmotic demyelination syndrome (ODS). This damages brain cells and can lead to permanent paralysis, difficulty speaking, or locked-in syndrome. It’s rare but devastating. That’s why doctors monitor sodium closely and avoid aggressive correction-even if you feel worse.
Next Steps: What to Do Now
If you’re on Natrise and worried about cost or side effects, ask your doctor about urea or demeclocycline. Bring up the studies. Ask if you can switch after a few weeks.
If you’re just starting out, don’t jump to drugs. Try fluid restriction for 7-10 days. If sodium doesn’t budge, then consider alternatives.
And if you’re in a hospital with low sodium and confusion? Make sure your team knows the correction limits. Ask: ‘What’s the plan to avoid raising sodium too fast?’
Hyponatremia isn’t just about numbers. It’s about quality of life. The right treatment doesn’t just fix sodium-it gives you back your energy, your clarity, your life.





Sherri Naslund
November 20, 2025 AT 06:16Ashley Miller
November 20, 2025 AT 11:20Martin Rodrigue
November 21, 2025 AT 00:49Brad Samuels
November 21, 2025 AT 11:08Mary Follero
November 22, 2025 AT 13:54Will Phillips
November 24, 2025 AT 02:40Arun Mohan
November 25, 2025 AT 16:17Tyrone Luton
November 26, 2025 AT 00:29