When someone in your family has had breast, ovarian, colon, or uterine cancer at a young age, it’s natural to wonder: is this hereditary? Genetic testing for cancer risk isn’t science fiction anymore-it’s a real, life-changing tool available today. For people with inherited mutations like BRCA1, BRCA2, or Lynch syndrome genes, knowing their risk isn’t just about fear-it’s about power. Power to prevent cancer before it starts. Power to catch it early. Power to choose treatments that actually work.
What BRCA and Lynch Really Mean
BRCA1 and BRCA2 aren’t just letters. They’re genes that normally help repair damaged DNA. When they’re broken by an inherited mutation, cells can’t fix errors properly. That’s when cancer starts to grow. A person with a harmful BRCA1 mutation has up to a 72% chance of getting breast cancer by age 80. For BRCA2, it’s about 69%. Compare that to the average woman’s 13% risk. Ovarian cancer risk jumps from 1.3% to 44% with BRCA1 and 17% with BRCA2. These aren’t small numbers.
Lynch syndrome is different. It’s caused by mutations in genes like MLH1, MSH2, MSH6, PMS2, or EPCAM. People with Lynch don’t just get colon cancer-they get it young, often before 50. Lifetime risk? Between 10% and 80%, depending on which gene is affected. They’re also at higher risk for uterine, ovarian, stomach, and even brain cancers. In fact, up to 80% of women with Lynch will develop some form of cancer by age 70.
These aren’t rare. About 1 in 400 people carry a BRCA mutation. Lynch syndrome affects roughly 1 in 280. That means in a room of 100 people, at least one person carries one of these mutations-and most don’t know it.
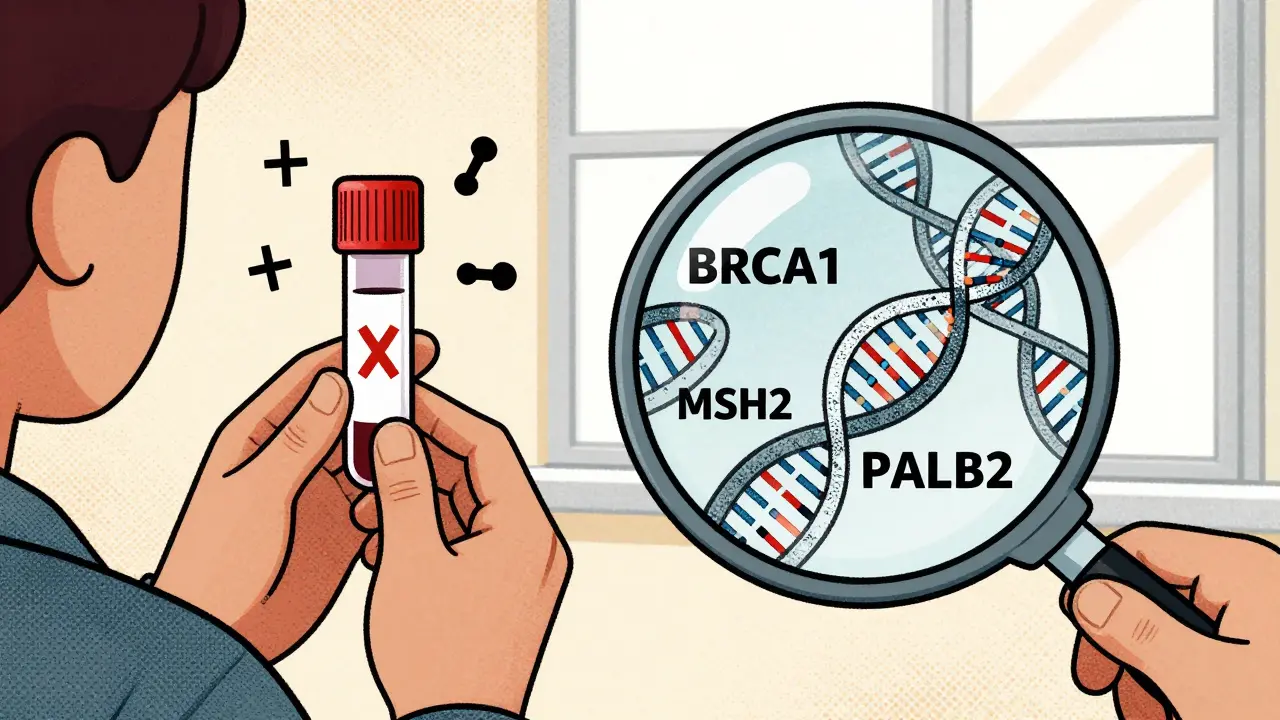
How Testing Works Today
Testing used to mean testing one gene at a time. If your doctor suspected BRCA, you got a BRCA test. If they thought Lynch, you got a Lynch panel. That’s outdated. Today, the standard is multigene panel testing (MGPT). A single blood or saliva sample can check 30 to 80+ cancer-related genes at once. Companies like Myriad, Invitae, and Color use next-generation sequencing (NGS), which reads your DNA with 99.5% accuracy for single-letter changes and 95% for large deletions or duplications.
The test doesn’t just look for BRCA or Lynch. It scans for mutations in PALB2, ATM, CHEK2, and others that also raise cancer risk. In 2025, the National Comprehensive Cancer Network (NCCN) added PALB2 and ATM to its top-tier list because they’re now proven to need action-just like BRCA.
Results come back in 14 to 21 days. But here’s the catch: not every change in your DNA is dangerous. About 7.8% of people who get a multigene panel test get a result labeled “variant of uncertain significance” (VUS). That means scientists don’t yet know if it causes cancer. It’s a gray zone. But progress is fast. In February 2025, researchers at Mayo Clinic used CRISPR to test nearly 7,000 BRCA2 variants. They cleared up 91% of the unknowns. That means fewer VUS results-and more certainty-for people tested today.
What the Tests Don’t Tell You
Not all genetic tests are equal. If you’ve seen those direct-to-consumer ads from 23andMe, you might think you’ve been tested. But their FDA-authorized BRCA test only looks for three specific mutations common in people of Ashkenazi Jewish descent. It misses over 97% of harmful BRCA mutations in everyone else. A negative result from 23andMe doesn’t mean you’re safe. It just means you didn’t get those three variants.
Whole-genome sequencing can read your entire DNA-99.99% accurate-but it’s expensive ($1,850) and brings back way more uncertain results. A 14.7% VUS rate means nearly 1 in 7 people get confusing news. That’s why most doctors stick with targeted panels. They’re cheaper ($250-$500), focused, and more likely to give clear answers.
And here’s something many don’t realize: a negative test doesn’t guarantee you won’t get cancer. If your family has a strong history but your panel test comes back negative, you could still have a mutation in a gene not yet tested-or one that current technology can’t detect. That’s why doctors always look at your family history, not just your results.
What Happens After a Positive Result
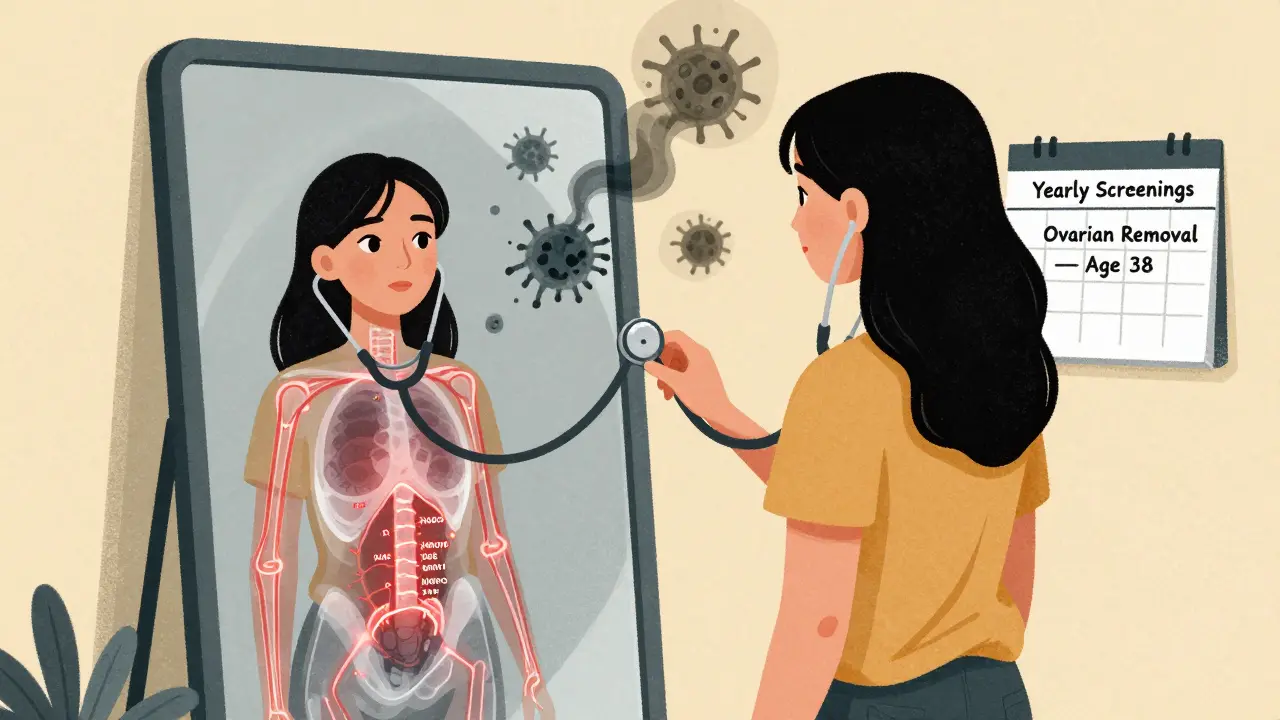
Getting a positive result isn’t the end. It’s the beginning of a plan. For BRCA carriers, options include:
- Starting breast cancer screening at age 25 with annual MRI and mammograms
- Considering risk-reducing mastectomy (removing breasts before cancer forms)-which cuts breast cancer risk by up to 90%
- Removing ovaries and fallopian tubes between ages 35-40, which cuts ovarian cancer risk by 80% and breast cancer risk by 50%
For Lynch syndrome, it’s about colon surveillance:
- Colonoscopies every 1-2 years starting at age 20-25
- Annual endometrial biopsies for women
- Aspirin taken daily, which studies show can cut colon cancer risk by up to 60%
And here’s the breakthrough: if you already have cancer, knowing your mutation changes your treatment. A 2025 case study from Fred Hutchinson Cancer Center showed a 42-year-old with colorectal cancer and Lynch syndrome responded completely to immunotherapy (pembrolizumab). That wouldn’t have happened if they didn’t know their mutation. Genetics now guides therapy-not just prevention.
The Hidden Challenges
Testing isn’t perfect. A 2024 JAMA study found that 18.7% of variant classifications differed between labs. That’s dangerous. One lab says “pathogenic,” another says “likely benign.” The same person gets two different stories. Thankfully, groups like ClinGen have created shared standards. They’ve reclassified over 1,200 BRCA variants since 2023. Discordance is now down to 8.3% for BRCA genes.
Insurance is another hurdle. Medicare covers testing if you meet NCCN criteria-and approves 98.7% of requests. But private insurers? Not always. A Reddit thread in January 2025 had 43 people reporting denials for testing their relatives, even though NCCN guidelines say cascade testing (testing family members after a positive result) is standard care.
And then there’s the cost. Even with insurance, out-of-pocket fees for testing can hit $450. And if you get a VUS? Some labs charge $250 to reanalyze your data later. Myriad’s patient portal has 78% positive reviews-but 32% of users complain about those reclassification fees.
Psychological impact is real, too. A 2024 survey found 22% of people felt major anxiety after a VUS result. Nine percent reported insurance discrimination-even though GINA (the Genetic Information Nondiscrimination Act) bans it. It still happens.
Who Should Get Tested?
You don’t need to be sick to qualify. The NCCN recommends testing if you have:
- Breast cancer diagnosed before age 45
- Ovarian, fallopian tube, or primary peritoneal cancer at any age
- Two or more close relatives with breast, ovarian, pancreatic, or aggressive prostate cancer
- Colon or uterine cancer before age 50
- A known mutation in your family
Even if you don’t have cancer, but your family does, you might still be eligible. A 2025 study found that 37% of people who tested positive for BRCA or Lynch had no prior cancer diagnosis. They were tested because of their family history-and now they’re protected.
But population-wide screening? Not yet. The American Society of Clinical Oncology warns it would flood the system with VUS results and cause more harm than good. Testing is targeted for a reason.
The Future Is Here
The field is moving fast. Researchers at Stanford identified 380 DNA variants that control how genes turn on and off in 13 cancers. These aren’t mutations-they’re switches. In the next decade, tests may combine your BRCA status with these switches to give you a personalized cancer risk score.
And soon, all cancer patients may be tested. A 2025 ASCO survey found 67% of oncologists support universal germline testing at diagnosis. Why? Because it changes treatment. It helps families. It saves lives.
But access isn’t equal. In academic centers, 48% of eligible patients get tested. In community clinics? Only 21%. And Black patients are tested at less than half the rate of white patients. That gap isn’t just unfair-it’s deadly.
Genetic testing isn’t magic. But when used right, it’s the closest thing we have to a cancer shield. It doesn’t stop bad luck. But it lets you turn bad luck into preparedness.
Is genetic testing covered by insurance?
Yes-if you meet clinical criteria. Medicare approves 98.7% of requests that follow NCCN guidelines. Most private insurers cover testing for people with personal or family histories of early-onset cancer. But some deny coverage for testing relatives (cascade testing), even though it’s recommended. Always check with your insurer before testing.
Can I get tested if I don’t have cancer?
Absolutely. In fact, that’s when testing is most powerful. If you have a strong family history of breast, ovarian, colon, or uterine cancer, testing before you get sick lets you prevent cancer entirely. Risk-reducing surgeries and enhanced screening can cut cancer risk by up to 80%.
What if my test shows a VUS?
A variant of uncertain significance (VUS) means scientists don’t know if it causes cancer. Don’t make medical decisions based on it. You should be managed based on your personal and family history, not the VUS. Many VUS results get reclassified over time. Ask your genetic counselor to recheck your result every 1-2 years.
Do direct-to-consumer tests like 23andMe work?
Only for a tiny subset. 23andMe’s test detects only 3 BRCA mutations common in Ashkenazi Jewish people. It misses over 97% of harmful mutations in everyone else. A negative result doesn’t mean you’re safe. Clinical testing through a doctor is the only reliable option.
Can genetic testing help if I already have cancer?
Yes. Knowing your mutation can change your treatment. BRCA carriers with ovarian or breast cancer may benefit from PARP inhibitors. Lynch syndrome patients with colorectal cancer often respond dramatically to immunotherapy. Testing after diagnosis can guide therapy and help your family avoid cancer too.