When your doctor prescribes a medication and your insurance says no, it’s not just frustrating-it can be dangerous. You’re stuck between a prescription you need and a system that’s designed to delay, not help. In 2024, prior authorization denials happened to 6% of all specialty drug requests in the U.S., but here’s the thing: 82% of those denials get overturned if you appeal. That means if you’re denied, you’re not out of luck-you’re just one step away from getting your medicine. Most people don’t appeal because they don’t know how. This guide walks you through exactly what to do, step by step, with real-world examples and insider tips that actually work.
Understand Why You Were Denied
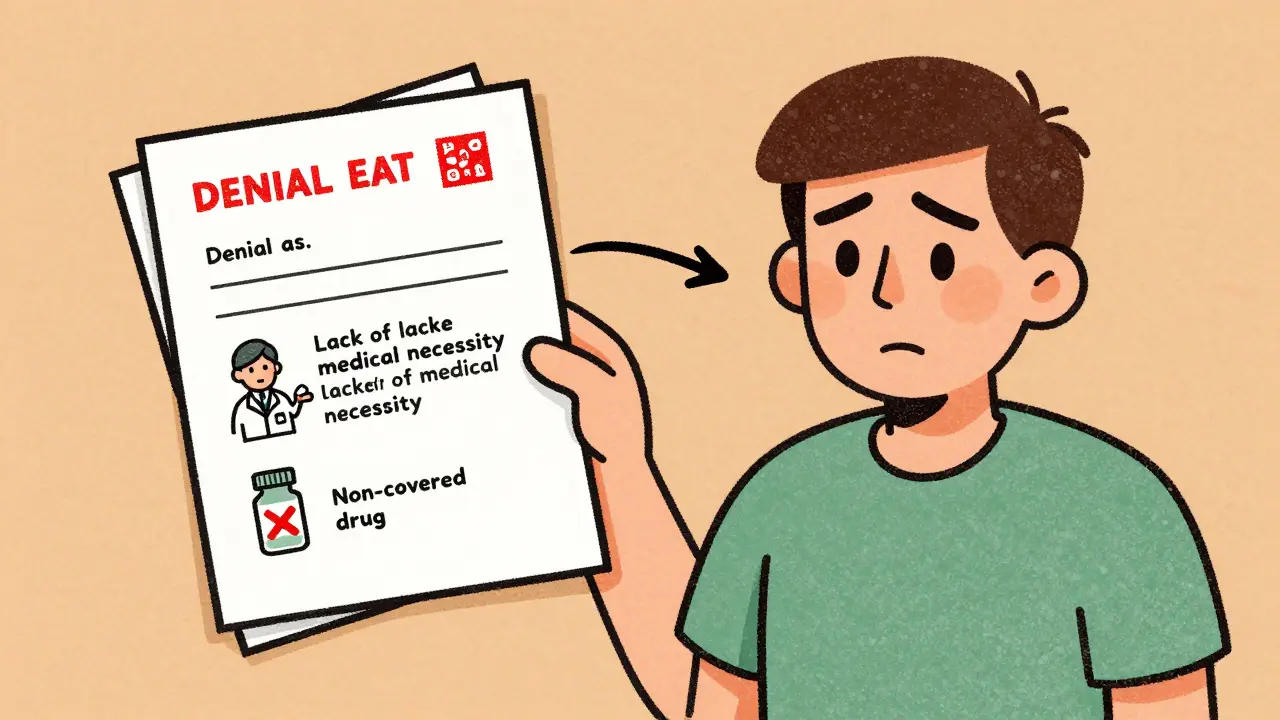
The first thing you need to do is read your denial letter. Don’t just glance at it. Underline the reason. Insurance companies don’t deny medications randomly. They have specific rules, and your denial falls into one of three buckets:- 37% are denied for incomplete paperwork-missing forms, wrong patient ID, or a form that wasn’t signed.
- 48% are denied for lack of medical necessity-the insurer thinks another drug should be tried first, even if your doctor says it won’t work.
- 15% are denied because the drug isn’t covered-it’s not on their formulary, or it’s restricted to certain conditions.
For example, if you were denied Humira for rheumatoid arthritis, the letter might say, “Alternative therapy preferred.” That doesn’t mean you can’t get it. It means they want proof that cheaper drugs failed first. If your doctor didn’t document that, you’re stuck. But if you have records showing you tried methotrexate for six months and your symptoms got worse? That’s your key.
Gather Every Piece of Paper
You’re not just appealing-you’re building a case. Insurers like CVS/Caremark and UnitedHealthcare require specific documents. Missing one thing can sink your appeal before it starts.Here’s what you need:
- A copy of the denial letter (always keep the original)
- Your full name, date of birth, insurance ID number
- Prescription details: drug name, dose, quantity, NDC number
- Medical records showing diagnosis (ICD-10 code)
- Lab results, progress notes, or test reports proving your condition
- A letter from your doctor explaining why this drug is necessary and why alternatives failed
- Proof of prior treatment failures-dates, names of drugs tried, side effects, outcomes
One patient on Reddit reversed a Humira denial in seven days because they included a two-page timeline of every failed medication, with exact dates and doctor notes. Another failed because they didn’t include the CPT code mentioned in the denial. Details matter. Don’t assume your doctor will send everything. Call their office. Ask them to print and sign a letter that says: “Patient has tried and failed at least two first-line therapies. This medication is medically necessary to prevent disease progression.”
Follow the Exact Appeal Process
Every insurer has its own rules. You can’t just email or call and expect results. You have to follow their procedure.Check your insurance’s website. Look for “Prior Authorization Appeal” or “Member Services.” Most require you to:
- Submit your appeal in writing
- Use their official form (if they have one)
- Send it by certified mail or through their online portal
- Meet the deadline: usually 180 days from the denial date
CVS/Caremark requires faxing to 1-888-836-0730. UnitedHealthcare forces you to use their online portal. If you send it the wrong way, they’ll reject it without review. Pro tip: If you’re unsure, call the provider relations department. They handle these appeals daily. Ask: “What’s the correct method to submit a prior auth appeal for [drug name]?” Most of the time, they’ll give you the exact form and address. That cuts out guesswork.
Write a Clear, Evidence-Based Appeal Letter
Your letter isn’t a plea. It’s a clinical argument. The goal is to match your evidence to the insurer’s own coverage rules.Here’s the structure that works:
- Start with your full name, ID, date of birth, and the drug you’re appealing.
- State the denial reason exactly as written in the letter.
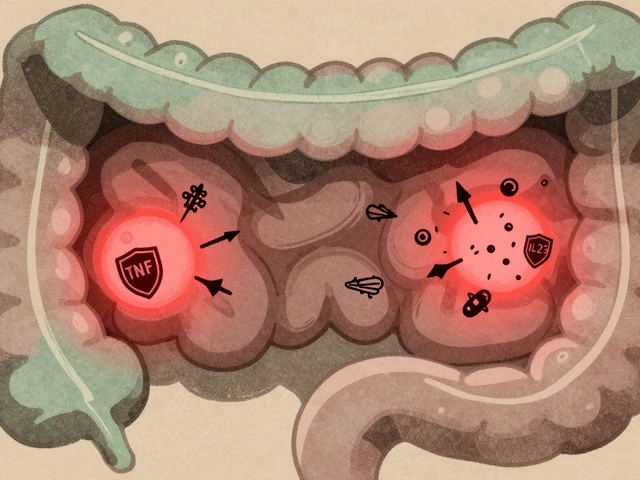
- Address each point with clinical evidence. For example: “The denial states ‘alternative therapy preferred.’ However, I have tried and failed on [Drug A] for 6 months with no improvement, and [Drug B] caused severe rash and hospitalization.”
- Include your diagnosis code (ICD-10) and the drug’s NDC code.
- Attach your doctor’s letter and supporting documents.
- End with: “I request immediate approval of this medication as it is medically necessary and aligned with your plan’s coverage criteria.”
Dr. Sonali Patel at Keck Medicine says appeals that directly quote the insurer’s own formulary guidelines have an 85% success rate. Don’t say, “This drug saves lives.” Say, “Per your 2024 Formulary Guidelines, Section 4.2, this medication is approved for patients with confirmed failure of two TNF inhibitors. Patient has failed adalimumab and etanercept.” That’s how you win.
Get Your Doctor Involved
Your doctor isn’t just a name on the form-they’re your strongest weapon. Insurers listen to doctors more than patients. But most doctors are overwhelmed. You have to ask them to help.Ask your doctor to:
- Write a letter that’s specific, not generic
- Include exact dates of failed treatments
- Reference the insurer’s own coverage policy
- Call the insurer’s medical review team directly
Keck Medicine’s 2024 data shows appeals with direct physician-to-insurer phone calls have a 32% higher success rate. Your doctor doesn’t need to spend hours. A 10-minute call to the medical director can clear up confusion faster than a stack of paperwork. If your doctor says no, ask for a nurse or medical assistant who handles prior auths. They do this all day.
Track Everything and Follow Up
Once you submit your appeal, don’t wait. Track it. Insurers say they’ll respond in 30 days, but 78% of physicians report needing multiple calls to get a response.Keep a log:
- Date you submitted
- Method used (fax, mail, portal)
- Confirmation number
- Name of person you spoke to
- Next follow-up date
Call after 14 days. Ask: “Has my appeal been reviewed? Can you give me a status update?” If they say “no decision yet,” ask for a supervisor. If they say “denied again,” you move to the next step.

Request an External Review
If your appeal is denied again, you have the right to an external review. This means an independent third party reviews your case-not your insurer.You have 365 days from the final denial to request this. The process varies by state, but most require:
- A written request
- Copy of your appeal and denial letters
- Medical records
External reviews reverse denials in 67% of cases. They’re your last line of defense-and they’re free. Medicare Advantage plans have faster external review timelines than commercial insurers. If you’re on Medicare, you’re in a better position.
What If You Still Get Denied?
If every step fails, you have options:- Ask for a patient assistance program-Many drug manufacturers (like AbbVie for Humira) offer free or low-cost medication if you’re denied insurance coverage.
- Use a pharmacy advocate-Some hospitals and nonprofits have staff who help patients navigate appeals for free.
- File a complaint with your state insurance department-They can pressure insurers to act. In 2023, 41% of denials were due to administrative errors-easily fixable if someone’s watching.
Don’t give up. The system is broken, but it’s not unbeatable. The average appeal takes 6-8 hours of your time. But if you get your medication, that time is worth it. One patient in Texas got her $12,000/month drug approved after three appeals. She said, “I didn’t know I could do this. Now I know: if you don’t fight, you lose.”
What’s Changing in 2026?
The system is slowly improving. In 2024, CMS mandated that Medicare Advantage plans respond to prior auth requests in 72 hours-down from 14 days. That’s cutting appeal needs by 18%. The CAQH Prior Authorization Clearinghouse, launching in 2025, will standardize forms across insurers, reducing errors by 27%. But until then, you still have to do the work. Don’t wait for the system to fix itself. Fix it for yourself.What should I do if my insurance denies my medication?
First, read the denial letter carefully to understand the reason. Then gather all medical records, your doctor’s letter, and proof of prior treatment failures. Submit a formal written appeal within 180 days using the insurer’s required method-whether it’s fax, mail, or online portal. Make sure your appeal directly addresses the denial reason with clinical evidence.
How long does a prior authorization appeal take?
Insurers are required to respond within 30 days for standard appeals. If your condition is urgent, you can request an expedited review, which must be decided within 72 hours. If your appeal is denied, you can request an external review, which takes up to 60 days for non-urgent cases and 72 hours for urgent ones.
Can my doctor help me appeal a denial?
Yes, your doctor is critical. They need to write a detailed letter explaining why the medication is medically necessary, list failed alternatives with dates and outcomes, and reference the insurer’s own coverage policy. Many insurers will even accept a direct phone call from the doctor’s office to the medical review team, which increases approval chances by 32%.
What if my appeal is denied again?
You have the right to an external review by an independent third party. Request this within 365 days of the final denial. You’ll need your denial letters and medical records. External reviews reverse denials in 67% of cases. You can also contact your state insurance department or ask the drug manufacturer for patient assistance programs.
Are prior authorization denials common?
Yes. About 6% of all prior authorization requests are denied each year, which adds up to nearly 19 million denials. But 82% of those denials are reversed when appealed. Most denials happen because of paperwork errors or lack of documentation-not because the drug isn’t needed. You’re not alone, and you’re not out of options.
Can I get my medication while I appeal?
Sometimes. Ask your doctor if they can request a temporary exception or a one-time supply while your appeal is pending. Some insurers allow this for life-threatening conditions. You can also ask the drug manufacturer for a patient assistance program or short-term free sample. Don’t wait-start these conversations as soon as you’re denied.
If you’ve been denied a medication you need, remember: you’re not powerless. The system is stacked against you, but the data doesn’t lie-appeals work. You’ve got the right to your medicine. Use it.



Laura Rice
January 23, 2026 AT 08:41I just got denied for my biologic last month-and I almost cried in the pharmacy parking lot. But then I remembered this guide. I printed out every lab result, made my doctor sign a letter that literally said, 'She’s been on methotrexate for 14 months and her CRP is still 18.' I faxed it to CVS Caremark using the number in the guide. Three days later, approval. I’m not crying anymore-I’m just mad I didn’t do this sooner.
Andrew Smirnykh
January 24, 2026 AT 02:13Interesting data. The 82% reversal rate is compelling, but I wonder how much of that is due to administrative errors versus clinical justification. In my experience with Medicare Advantage, many denials stem from coding mismatches-like when the ICD-10 code doesn’t align perfectly with the drug’s approved indication, even when the clinical picture is clear. It’s less about the patient’s need and more about the system’s rigidity.
charley lopez
January 24, 2026 AT 07:56The prior authorization process remains a non-value-added administrative burden that introduces significant friction into the clinician-patient therapeutic alliance. Per CMS guidelines, the 72-hour turnaround mandate for Medicare Advantage plans represents a step toward streamlining, yet the variance in payer-specific formularies and submission protocols continues to engender inefficiencies. Optimal outcomes require standardized digital interoperability, which CAQH aims to address.
Kerry Evans
January 25, 2026 AT 12:24People complain about denials, but half the time they don’t even follow the basic steps. I’ve seen patients skip the doctor’s letter, miss the fax number, and then blame the insurance. It’s not the system-it’s the lack of effort. If you can’t be bothered to read the denial letter or call your doctor’s office, don’t act surprised when you get denied again. This guide is good, but it’s not magic. You have to do the work.
Kerry Moore
January 26, 2026 AT 02:25Thank you for this comprehensive and meticulously structured resource. The inclusion of specific insurer protocols, documentation checklists, and the emphasis on physician advocacy are particularly valuable. I would like to respectfully suggest that a supplementary appendix listing state-specific external review procedures may further enhance accessibility for patients navigating regional regulatory differences.