Why Patients Think Generics Don’t Work - Even When They Do
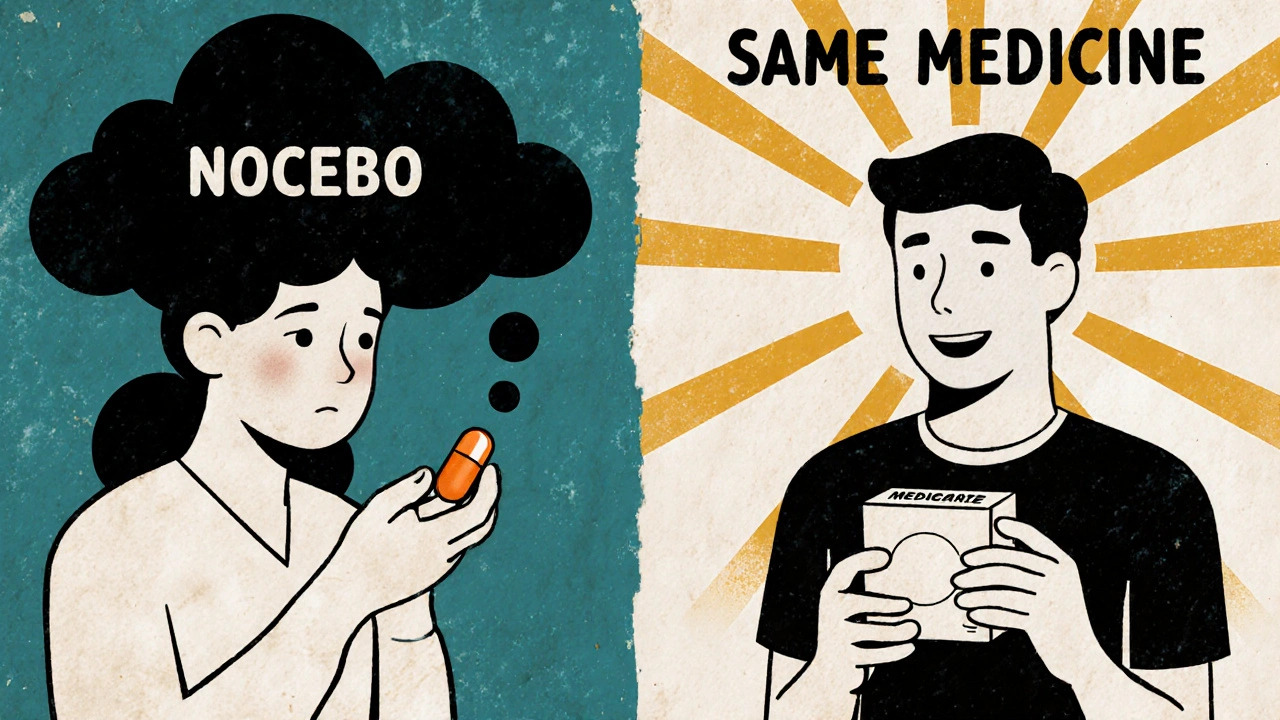
Imagine switching from your brand-name antidepressant to the generic version, only to start feeling worse. Headaches. Fatigue. Nausea. You didn’t have these before. Your doctor says it’s the same drug. But your body feels different. You’re not imagining it - and you’re not alone.
More than 89% of prescriptions filled in the U.S. are for generic drugs. Yet nearly 4 in 10 patients still believe generics are less effective or more likely to cause side effects. This isn’t about chemistry. It’s about perception. And that perception is triggering something real: the nocebo effect.
The nocebo effect isn’t a myth. It’s a measurable, repeatable phenomenon where negative expectations turn harmless substances into sources of harm. In one 2025 study, healthy people given a fake nasal spray labeled as a generic - with a complex name and low price - reported more side effects than those given the exact same placebo labeled as a brand-name product. Even though neither contained any active ingredient, the generic label made people feel worse. That’s the power of belief.
How the Nocebo Effect Works - And Why It Hits Generics Harder
When you’re told a drug might cause dizziness, nausea, or mood swings, your brain starts scanning for those sensations. Normal fatigue? Must be the pill. A mild headache? Probably the generic. This isn’t weakness. It’s how your mind works. Your brain doesn’t distinguish between real and expected symptoms - it just reacts.
Generics get hit hardest because of three things: packaging, price, and naming.
Take a 2024 study where participants used a fake anti-itch cream. One group got it in a sleek blue box with the name “Solestan® Creme.” The other got the same cream in a plain orange box labeled “Imotadil-LeniPharma Creme.” The group with the cheap-looking packaging reported more pain - even though the cream had no active ingredient. Price isn’t just about cost. It’s a signal. Expensive = effective. Cheap = risky.
Same thing happens with names. A generic pill labeled “Sertraline Hydrochloride 50 mg” sounds clinical, intimidating. The brand version, “Zoloft,” sounds familiar, trusted. When patients switch, their brain doesn’t see the same drug. It sees a different one.
And it’s not just patients. Doctors, pharmacists, and even media reports can unintentionally reinforce these beliefs. A 2017 change in New Zealand from one brand of venlafaxine to a generic saw no spike in side effect reports - until local news ran stories about “generic switch problems.” Then reports jumped 300%.
What Science Says: Generics Are Just as Safe and Effective
Let’s cut through the noise. Generics aren’t cheaper because they’re lower quality. They’re cheaper because they don’t need to repeat expensive clinical trials. The U.S. Food and Drug Administration (FDA) requires generics to meet the same strict standards as brand-name drugs: same active ingredient, same dose, same strength, same way of being absorbed.
For a generic to be approved, it must deliver the same amount of medicine into your bloodstream - within 80% to 125% of the brand-name version. That’s not a guess. That’s science. And it’s backed by over 1,000 bioequivalence studies every year.
A 2021 meta-analysis of 37 studies found that while patients report more side effects after switching to generics, the actual clinical outcomes - like blood pressure control, seizure frequency, or depression scores - are identical. The difference? Perception, not pharmacology.
Even when generics come from the same factory as the brand-name drug - called “authorized generics” - patients still report more side effects. That’s the nocebo effect in action. The pill is the same. The box is different. And that’s enough to change how you feel.

How Healthcare Providers Can Reduce the Nocebo Effect
Changing how you talk about generics can change how patients respond.
Here’s what works:
- Don’t lead with risks. Instead of saying, “This generic might cause dizziness, nausea, or insomnia,” say, “Most people tolerate this medication just as well as the brand. You’re getting the same medicine, just at a lower cost.”
- Use trusted language. Say, “This is the exact same active ingredient as your previous medication.” Avoid words like “substitute” or “alternative.” Those imply difference.
- Highlight savings. A 2022 study showed that when patients were told switching to a generic could save them over $3,000 a year - and that the effectiveness was the same - nocebo effects dropped by 37%.
- Normalize the switch. “Many patients switch to generics without any issues. If you notice anything unusual, we’ll adjust together.” This frames the change as routine, not risky.
- Don’t ignore concerns. If a patient says, “I felt worse after the switch,” don’t dismiss it. Say, “That’s actually more common than you think - it’s not the drug, it’s your brain expecting side effects. Let’s see if we can reframe this.”
Some clinics, like Kaiser Permanente, now use standardized scripts for generic switches. One example: “This medication contains the exact same active ingredient as what you were taking before. Studies show patients do just as well on the generic version. If you notice any changes, we’ll work on them together.”
What Patients Can Do to Protect Themselves
You don’t have to be passive in this. Here’s how to take control:
- Ask: “Is this the same as my old pill?” If yes, remind yourself: same chemistry, same effect.
- Track symptoms objectively. Use a simple journal: rate your fatigue, headaches, or mood on a scale of 1-10 before and after the switch. Often, you’ll see no real change.
- Check the source. If you’re reading about side effects on Reddit or Facebook, remember: people report problems more than they report success. The quiet majority doesn’t post.
- Don’t assume cost = quality. A $5 generic isn’t a “cheap version.” It’s a scientifically proven copy.
- Give it time. The nocebo effect often fades after 2-4 weeks as your brain adjusts. Don’t rush back to the brand unless symptoms are truly new and severe.
Why Packaging and Branding Matter More Than You Think
Look at the pill in your hand. The color, the shape, the imprint - they’re not random. They’re designed to trigger trust or suspicion.
Some manufacturers now make “branded generics” - generics that look and feel like the original brand. Same size. Same color. Same logo. These have lower nocebo rates because they reduce the psychological shock of switching.
But here’s the catch: the European Medicines Agency says packaging shouldn’t mimic brand-name products to avoid confusion. So there’s a tension between safety and perception.
For now, the best solution is transparency. If your pharmacy changes the pill you’ve been taking, they should tell you - not just on a sticker, but in person. And they should explain: “This is the same medicine. The only difference is the name on the box.”
What’s Next? Better Tools, Better Conversations
Researchers are now building tools to spot who’s most vulnerable to nocebo effects. The Beliefs about Medicines Questionnaire (BMQ) asks things like: “Do you worry that medications do more harm than good?” People who score high on worry are more likely to report side effects - even with placebos.
Future studies are using fMRI scans to see how the brain reacts when people think they’re taking a generic. Early results show increased activity in areas linked to fear and pain anticipation.
Public health campaigns are starting too. In Australia, the Therapeutic Goods Administration has begun pilot programs showing patients side-by-side comparisons of brand and generic pills - with the same active ingredient highlighted in bold. Early feedback? Fewer complaints, more trust.
The goal isn’t to trick patients. It’s to give them the truth - in a way that doesn’t trigger fear.
Final Thought: The Real Difference Isn’t in the Pill - It’s in the Mind
Generics aren’t second-rate. They’re second-generation - better because they’re proven, cheaper, and just as safe.
The nocebo effect is real. But it’s not inevitable. With the right conversation, the right framing, and the right timing, patients can make the switch without fear.
You’re not getting less. You’re getting the same - just without the brand markup. And that’s not just smart economics. It’s smart medicine.
Do generic medications have the same active ingredients as brand-name drugs?
Yes. By law, generic medications must contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. The FDA and other global regulators require proof that the generic delivers the same amount of medicine into your bloodstream at the same rate - within a strict 80-125% range. The only differences are in inactive ingredients like fillers, colors, or packaging - none of which affect how the medicine works.
Why do I feel worse after switching to a generic?
You’re likely experiencing the nocebo effect - not a problem with the drug itself. When you expect side effects, your brain becomes more sensitive to normal bodily sensations like fatigue or mild headaches. Studies show people report more side effects when they believe they’re taking a cheaper or less trusted version - even when the pill is identical. This isn’t in your head in a fake way; it’s a real psychological response that changes how you feel.
Are generics less effective for chronic conditions like depression or epilepsy?
No. Large studies, including reviews by the Annals of Internal Medicine and PLOS Medicine, show no difference in effectiveness for chronic conditions when switching to generics. For depression, epilepsy, hypertension, and diabetes, clinical outcomes are identical between brand and generic versions. The only variation comes from patient perception - not the medicine’s performance.
Can packaging really affect how I feel on a medication?
Yes. Research has shown that the color, shape, and branding of a pill or its packaging can influence side effect reporting - even when the medicine inside is identical. In one study, people using a fake cream in a sleek blue box reported more pain than those using the same cream in a plain orange box. This isn’t placebo; it’s nocebo. Your brain associates expensive-looking packaging with safety and effectiveness - and plain packaging with risk.
Should I ask my doctor to keep me on the brand-name drug?
Only if you’ve tried the generic and had real, persistent side effects that aren’t explained by the nocebo effect. Otherwise, switching to a generic is safe, effective, and saves money - often over $3,000 a year. If you’re worried, ask your doctor to explain the switch using clear, positive language. Many clinics now use scripts that reduce fear and increase trust. You don’t have to choose between cost and care - you can have both.



Brandon Lowi
November 19, 2025 AT 09:07Joshua Casella
November 21, 2025 AT 08:12Richard Couron
November 22, 2025 AT 16:41Alex Boozan
November 23, 2025 AT 04:09mithun mohanta
November 23, 2025 AT 11:13Evan Brady
November 25, 2025 AT 08:58Ram tech
November 26, 2025 AT 01:06Jenny Lee
November 27, 2025 AT 05:40Erica Lundy
November 27, 2025 AT 08:02Kevin Jones
November 28, 2025 AT 07:31