Immunosuppressant-Echinacea Interaction Checker
Check Your Medication Risk
Many people turn to echinacea when they feel a cold coming on. It’s one of the most popular herbal supplements in the world, sold in nearly every pharmacy and health store. But if you’re taking medication to suppress your immune system-after a transplant, for example, or because of an autoimmune disease like lupus or rheumatoid arthritis-echinacea could be putting your health at serious risk.
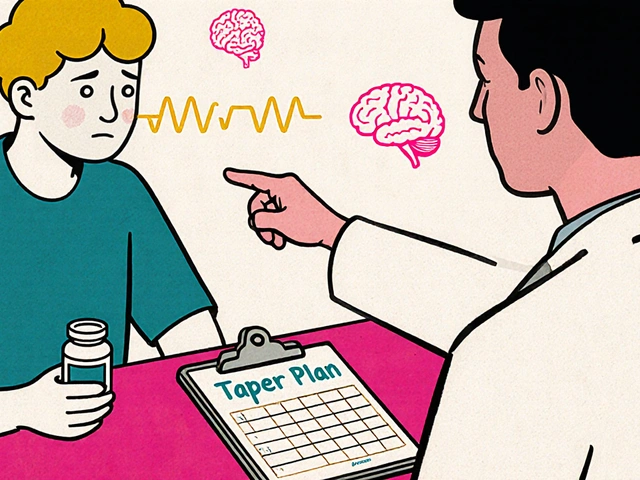
How Echinacea Works (And Why It’s a Double-Edged Sword)
Echinacea is made from the roots and flowers of plants in the daisy family. For decades, it’s been marketed as an immune booster. And in the short term, that’s mostly true. Studies show it activates white blood cells like neutrophils and macrophages, increases phagocytosis (the process where immune cells eat up invaders), and boosts natural killer cell activity. These are all good things when you’re fighting off a virus.
But here’s the catch: long-term use changes everything. After about eight weeks, research suggests echinacea may start doing the opposite. Instead of stimulating the immune system, it begins to suppress it. This flip-flop effect isn’t just confusing-it’s dangerous when combined with drugs designed to calm your immune response.
The active ingredients in echinacea-alkamides, polysaccharides, and caffeic acid derivatives-interact with receptors in your immune cells, including cannabinoid receptor type 2 (CB2). This is why it can both turn up and turn down immune activity. It’s not a simple on/off switch. It’s more like a dimmer that flickers unpredictably, especially with prolonged use.
What Are Immunosuppressants?
Immunosuppressants are powerful drugs that lower your body’s ability to attack foreign tissue. They’re essential for people who’ve had organ transplants-kidney, liver, heart, lung-because without them, your immune system would reject the new organ. They’re also used to treat autoimmune diseases like multiple sclerosis, Crohn’s disease, and psoriasis, where your body mistakenly attacks itself.
Common immunosuppressants include:
- Cyclosporine
- Tacrolimus
- Azathioprine
- Mycophenolate mofetil
- Methotrexate
- Corticosteroids (like prednisone)
These drugs work by targeting specific parts of the immune system. They’re finely balanced. Too little, and rejection or flare-ups happen. Too much, and you’re at risk for infections or cancer. That’s why even small changes-like adding a supplement-can throw things off.
The Real Risk: Echinacea vs. Immunosuppressants
When you take echinacea while on immunosuppressants, you’re essentially sending mixed signals to your body. Your medication is trying to quiet your immune system. Echinacea is trying to wake it up. The result? Your immune system doesn’t know what to do-and neither does your doctor.
There’s no large-scale clinical trial proving this interaction causes rejection every time. But that doesn’t mean it’s safe. In fact, the evidence against it is stronger than you might think.
Memorial Sloan Kettering Cancer Center has documented multiple case reports:
- A 55-year-old man with pemphigus vulgaris (a rare autoimmune skin disease) had a severe flare-up after starting echinacea. His immunosuppressant dose had to be increased, and he never fully recovered.
- A 61-year-old lung cancer patient developed life-threatening low platelet counts while taking echinacea alongside chemotherapy.
- A 32-year-old man developed thrombotic thrombocytopenic purpura (TTP), a rare and deadly blood disorder, after using echinacea for a cold.
These aren’t rare anomalies. They’re warning signs.
The American Society of Health-System Pharmacists classifies this interaction as “moderate”-meaning it’s not just a theoretical concern. It’s something that has caused real harm. And the American Society of Transplantation says it clearly: avoid echinacea completely if you’ve had a transplant.

Why Other Herbs Are Safer (And Why Echinacea Isn’t)
Not all herbal supplements behave the same way. Ginger, for example, has mild anti-inflammatory effects but doesn’t directly stimulate immune cells. Turmeric affects inflammation pathways, but not the same ones targeted by immunosuppressants. Milk thistle helps the liver, but doesn’t touch immune function.
Echinacea is different. It directly interferes with the very systems immunosuppressants are trying to control. That’s why it’s one of the few herbs that major medical organizations specifically warn against for transplant and autoimmune patients.
Even the European Medicines Agency and the U.S. FDA agree: the risk of interaction can’t be ruled out. In 2023, the FDA sent warning letters to three supplement makers for promoting echinacea as an immune booster without disclosing the danger to people on immunosuppressants.
What Patients Are Saying (And Why It Matters)
Online patient forums tell a troubling story. A 2022 analysis of 147 posts from transplant recipients found 23 cases where people suspected echinacea caused problems. Seventeen needed higher doses of their immunosuppressants. Six had acute rejection episodes.
And here’s the scary part: most of these patients didn’t tell their doctors they were taking echinacea. They assumed it was “natural,” so it must be safe. One woman wrote: “I didn’t think my transplant team would care about a little herbal tea.”
That’s a dangerous mindset. A 2021 Mayo Clinic survey of 512 transplant patients found 34% had used echinacea after their transplant. Twelve percent reported complications they believed were linked to supplements. Yet only a fraction of them had discussed it with their care team.

What Should You Do?
If you’re on immunosuppressants:
- Stop taking echinacea immediately. Even if you’ve been using it for months without issues, the risk is cumulative. The longer you take it, the higher the chance of interference.
- Tell your doctor about every supplement you take. Not just echinacea-vitamins, fish oil, probiotics, herbal teas. Your provider needs the full picture to manage your treatment safely.
- Don’t assume “natural” means safe. Natural doesn’t mean harmless. Many toxins in nature are also natural. Echinacea is a powerful plant compound, not a harmless tea.
- Ask for alternatives. If you’re using echinacea to prevent colds, talk to your doctor about safer options: handwashing, sleep, vitamin D, and flu shots are proven and safe.
The Cleveland Clinic and the American College of Rheumatology both recommend avoiding echinacea entirely if you’re on immunosuppressive therapy. That’s not a suggestion-it’s a medical guideline backed by decades of clinical observation and growing evidence.
What’s Being Done About It?
The National Institutes of Health is currently funding a $2.4 million study (NCT04851234) to see exactly how echinacea affects tacrolimus levels in kidney transplant patients. Results are expected in early 2025. This is the first major study of its kind.
In the meantime, EU countries now require echinacea labels to include warnings about immunosuppressant interactions. In the U.S., the FDA is cracking down on companies that make unproven claims without disclosing risks.
But until we have more data, the safest choice is clear: if you’re on immunosuppressants, don’t take echinacea. Not for a week. Not for a month. Not even for a cold.
Bottom Line
Echinacea might help your immune system fight a cold-but it can also make your transplant rejection or autoimmune flare-up worse. There’s no middle ground here. The science, the case reports, and the expert guidelines all point to the same conclusion: avoid echinacea if you’re taking immunosuppressants.
Your body is already working hard to stay healthy. Don’t let a supplement undo that work.




Kaitlynn nail
December 10, 2025 AT 16:37Echinacea? More like echin-danger. Nature doesn’t care about your PhD or your transplant. It just wants to confuse your cells. The body isn’t a machine you can tweak with herbal tea.
It’s a battlefield. And you just handed the enemy a grenade labeled 'natural'.
Michelle Edwards
December 11, 2025 AT 02:58I get it-you want to feel like you’re doing something proactive when you’re sick. But your body’s already doing so much. Let your meds do their job. You don’t need to 'boost' anything. Just rest. Drink water. Listen to your body.
You’re already stronger than you think.
Raj Rsvpraj
December 12, 2025 AT 10:43Of course, Americans think herbs are medicine-while we in India have been using Ayurveda for 5,000 years, and we know exactly what plants do! Echinacea? A Western placebo for people who can’t handle real science.
Also, your FDA is a joke. They let Big Pharma control everything-except when it suits them to scare you about 'natural' things.
Don’t be a sheep. Question the narrative.
Frank Nouwens
December 13, 2025 AT 14:05While the anecdotal evidence presented is compelling, it remains insufficient to establish a causal relationship between echinacea and immunosuppressant interactions without controlled, longitudinal data.
That said, the precautionary principle is ethically and clinically justifiable in this context, given the potential severity of outcomes.
Therefore, avoidance is not merely prudent-it is a standard of care.
Aileen Ferris
December 14, 2025 AT 18:22echinacea?? more like echin-nope lmao
also why is everyone so scared of plants?? i drink chamomile tea and i’m fine. also my cat eats grass. what’s the deal??
Nikki Smellie
December 15, 2025 AT 14:50They don’t want you to know this… but echinacea is a mind-control plant. The FDA and Big Pharma are terrified of it because it proves your immune system can heal itself without drugs. That’s why they scare you with ‘rejection’ stories.
They’re hiding the truth. You’re being manipulated. Your transplant team? They’re paid by the drug companies.
🌱 I took echinacea for 3 years. My labs improved. They didn’t tell you that, did they? 😔
Neelam Kumari
December 16, 2025 AT 15:31Wow. So you’re telling me someone actually believed a plant could 'boost' immunity? Did you get this advice from a yoga instructor who sells crystals? Or maybe a TikTok influencer with 12 followers?
People like you are why medicine is so broken.
Stop treating your body like a garden and start treating it like a biological system. You’re not a plant. You’re a human with a functioning immune system. And it doesn’t need your 'herbal tea' to 'feel loved'.
Queenie Chan
December 17, 2025 AT 17:05It’s wild how echinacea’s dual-phase effect mirrors the chaos of modern life-first you’re fired up, then you crash. It’s like your immune system’s doing a bad impression of a caffeine binge.
And yet, we’re still surprised when biology gets messy?
Maybe the real issue isn’t the herb-it’s that we treat our bodies like we treat our phones: plug in a new app, hope it fixes everything.
But the body doesn’t run on plugins. It runs on balance. And balance? That’s hard to sell in a 30-second ad.
Doris Lee
December 19, 2025 AT 07:22You’re not alone if you’ve taken echinacea without knowing. I did too. I thought it was harmless. But now I know better-and I’m so glad I found this post.
You’re not stupid for trying. You’re just human.
Now that you know, you’re already doing better. Keep going. You’ve got this.
Michaux Hyatt
December 19, 2025 AT 17:49For anyone on immunosuppressants: if you’re unsure about a supplement, ask your pharmacist. Not Google. Not your aunt. Not Instagram.
Pharmacists are the unsung heroes of medication safety. They know interactions better than most doctors because they see the whole picture-every pill, every tea, every tincture.
Walk in. Ask. No judgment. Just facts. You deserve that.
Rebecca Dong
December 20, 2025 AT 00:57Okay but what if I’m a witch? 🧙♀️
What if echinacea is my familiars’ favorite snack and my immune system is literally a dragon that only wakes up when I drink it?
What if the FDA is just scared of magic??
Also my cat sneezed after I took it. Coincidence? I think NOT.
Sarah Clifford
December 20, 2025 AT 17:17So… no echinacea. Got it. But what about elderberry? Is that also evil? Because I have a whole jar. 😅