When you hear the word radiation, you might think of X-rays at the dentist or nuclear accidents. But for millions of people with cancer, radiation is a lifeline. Radiation therapy doesn’t just zap tumors-it shatters the very blueprint that lets cancer cells survive and multiply. And understanding how it works changes everything about how we treat cancer today.
How Radiation Breaks Cancer Cells Apart
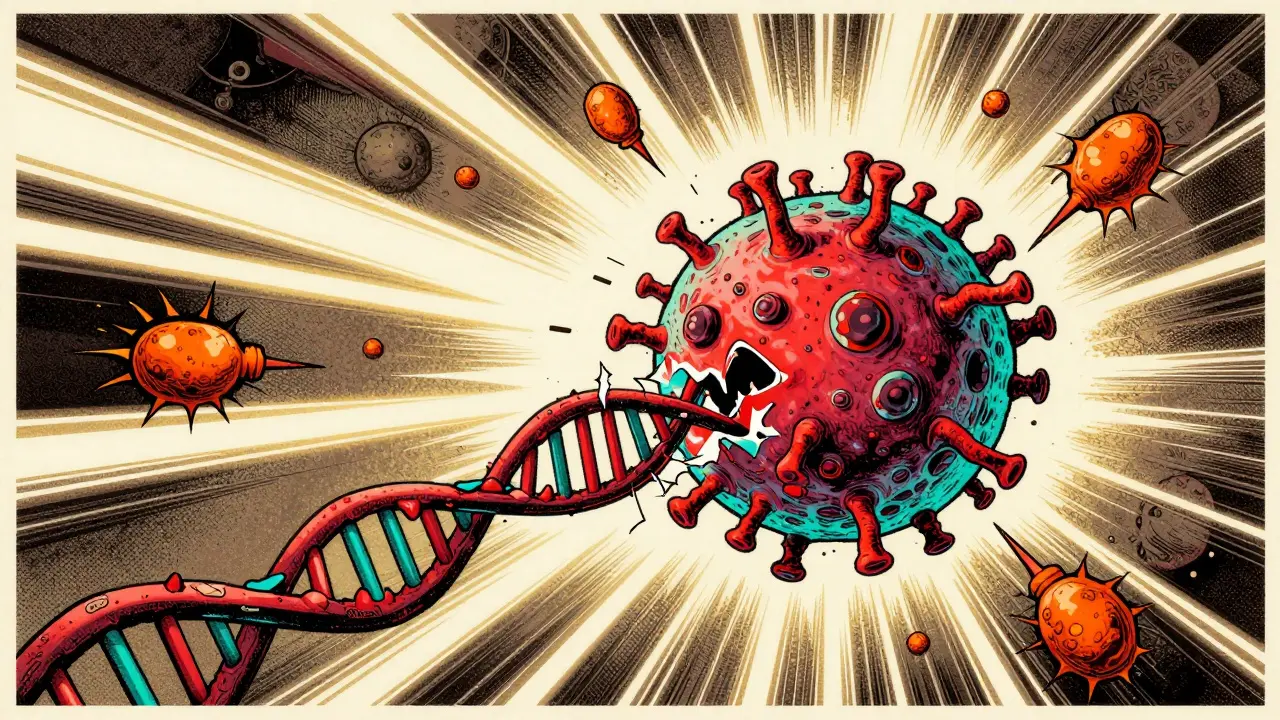
Radiation therapy uses high-energy particles or waves-usually X-rays or protons-to target cancer cells. The goal isn’t just to burn them. It’s to break their DNA. When ionizing radiation hits a cell, it doesn’t just nudge the DNA. It smashes it. The most dangerous kind of damage is a double-strand break, where both sides of the DNA ladder snap apart. Unlike a single strand break, which the cell can often fix, a double-strand break is like cutting both ends of a zipper. Without the right repair tools, the cell can’t copy itself properly.This is why radiation is so effective against fast-growing cancers. Tumors divide constantly, and every time a cancer cell tries to split, it needs its DNA intact. If the DNA is broken and not fixed in time, the cell either dies right away or gets stuck trying to divide-leading to what’s called mitotic catastrophe. The cell explodes during division, unable to complete the process. It’s messy, but it works.
The Two Main Ways Radiation Kills Cells
There are two primary paths radiation takes to kill cancer cells: direct damage and indirect damage.Direct damage happens when radiation hits DNA head-on. This is more common with heavier particles like protons. But in most cases, especially with standard X-ray therapy, the damage is indirect. Radiation hits water molecules inside the cell, splitting them into reactive oxygen species (ROS). These are like molecular grenades. They fly around, oxidizing proteins, wrecking cell membranes, and-most importantly-attacking DNA. This oxidative stress overwhelms the cell’s natural defenses.
Once the damage is done, the cell has a few options. It can try to repair itself. It can shut down and die quietly through apoptosis. Or it can keep trying to divide anyway and fall apart mid-process. The most common death route in solid tumors is reproductive failure-cells don’t die immediately. They just can’t make copies anymore. Over days or weeks, the tumor stops growing because no new cancer cells are being born.
How Cells Try to Fix the Damage (And Why That Matters)
Cells aren’t helpless. They have repair crews. Two main teams show up after radiation hits: non-homologous end joining (NHEJ) and homologous recombination (HR).NHEJ is the quick-and-dirty fix. It glues broken ends back together, no matter how messy. It’s fast but error-prone. That’s actually good in cancer treatment-because errors mean the cell can’t function anymore. HR, on the other hand, is the precision repair team. It uses a healthy copy of DNA as a template to fix the break perfectly. It’s accurate, but it takes time. And here’s the twist: cells that use HR often die without triggering any alarm bells. They vanish quietly during cell division.
But cells that can’t use HR-like those with BRCA2 mutations-don’t die quietly. They leak signals. They scream. They release molecules that look like viral invaders. That’s when the immune system wakes up. Instead of just removing dead cancer cells, the body starts hunting down the rest of the tumor. This is a game-changer. It means radiation isn’t just a local treatment. It can become a whole-body attack if the cancer cell’s repair system fails.
Why BRCA Mutations Change Everything
About 5 to 10% of breast cancers and 15 to 20% of ovarian cancers carry BRCA1 or BRCA2 mutations. These genes are essential for homologous recombination. When they’re broken, cancer cells can’t fix DNA properly. That makes them more sensitive to radiation-but not just because they die faster. They die differently.Research from the Cancer Medicine Research Institute (CMRI) showed that BRCA2-deficient cells don’t die during mitosis. Instead, they explode in a way that releases danger signals. This turns radiation into a vaccine-like trigger. The immune system learns to recognize those cancer cells as threats. And once trained, it keeps looking for them-even if they spread elsewhere.
This is why doctors are now combining radiation with immunotherapy. Drugs like pembrolizumab block the brakes on immune cells. When you add radiation to those drugs, the immune system doesn’t just respond-it multiplies its attack. In one trial, metastatic lung cancer patients saw their response rate jump from 22% to 36% when radiation was added to immunotherapy. That’s not a small gain. That’s a turning point.
The Role of Oxygen and the Tumor Environment
Radiation doesn’t work well in low-oxygen environments. Tumors often outgrow their blood supply, creating dead zones where oxygen levels are too low for radiation to be effective. In these hypoxic areas, cancer cells can survive doses that would kill cells in well-oxygenated tissue. In fact, hypoxia can make cells up to three times more resistant to radiation.That’s why some newer techniques focus on improving oxygen delivery or using drugs that mimic oxygen’s effects. Other approaches target the tumor’s support system. Cancer-associated fibroblasts and immune-suppressing cells around the tumor act like bodyguards for cancer cells. They shield them from radiation and help them repair damage. New treatments are now designed to break down these shields-making radiation more effective even in stubborn tumors.
How Modern Tech Makes Radiation Smarter
Gone are the days of broad beams that burned skin and damaged healthy organs. Today’s machines-like linear accelerators-can shape radiation beams to match the tumor’s exact 3D shape. Intensity-modulated radiation therapy (IMRT) adjusts the strength of the beam across different areas. Stereotactic body radiation therapy (SBRT) delivers high doses in just a few sessions with sub-millimeter precision.FLASH radiotherapy is the next frontier. It delivers the entire dose in less than a second-faster than a camera shutter. Early studies show it kills tumors just as well but causes far less damage to surrounding tissue. The first human trials started in 2020, and results are promising. If this scales up, it could mean fewer side effects and better quality of life during treatment.
Artificial intelligence is also stepping in. Treatment planning used to take hours. Now, deep learning algorithms can design a personalized radiation plan in under 10 minutes. These systems learn from thousands of past cases, predicting how a tumor will respond and adjusting doses in real time.

The Future: Radiation as a Catalyst
Radiation therapy is no longer just about killing cells. It’s about changing how the body sees cancer. By forcing cancer cells to die in ways that alert the immune system, we’re turning radiation into a trigger for systemic immunity. Combining it with drugs that block DNA repair-like PARP inhibitors-or boost immune response is already extending survival for patients with BRCA-mutated cancers.And it’s not just about the tumor. The way radiation affects blood vessels inside the tumor matters too. High-dose radiation can destroy the tiny vessels feeding the tumor, starving cancer cells days after treatment. This delayed effect, driven by the ceramide pathway, adds another layer to how radiation works.
What we’re seeing now is a shift from brute force to precision biology. Radiation isn’t just a scalpel. It’s a signal. It’s a teacher. It’s a partner to the immune system. And for patients who once saw radiation as a last resort, it’s becoming a cornerstone of cure.
Why Some Tumors Resist Radiation
Despite all the advances, about 30 to 40% of tumors don’t respond well. Why? Because cancer evolves. Some tumors overproduce repair proteins like 53BP1. One study found patients with head and neck cancer who had high levels of 53BP1 had a 45% chance of complete response to radiation. Those with low levels? 78%. That’s a huge difference. It means we can now test tumors before treatment to predict who will benefit most.Other resistance mechanisms include cells that pause their cycle to avoid radiation’s peak damage, or tumors that activate survival pathways like NF-kB. These are the next targets for drug development. The goal isn’t just to kill more cells-it’s to make sure the ones that survive can’t come back.
How long does it take for radiation to kill cancer cells?
Radiation doesn’t kill cancer cells instantly. Most cells die over days or weeks as they try to divide with damaged DNA. Some die during treatment, but the full effect often shows up weeks after the last session. Imaging scans usually don’t show tumor shrinkage until 4 to 8 weeks post-treatment.
Does radiation therapy hurt?
No, the treatment itself is painless, like getting an X-ray. But side effects like skin irritation, fatigue, or soreness in the treated area can develop over time. These are usually temporary and managed with supportive care.
Can radiation therapy cause cancer?
It’s possible, but extremely rare. Radiation therapy is carefully planned to minimize exposure to healthy tissue. The risk of developing a second cancer from treatment is less than 1% over 10 years-far lower than the benefit of curing the original cancer.
Why is radiation used with chemotherapy?
Chemotherapy weakens cancer cells and makes them more vulnerable to radiation. The two work together like a one-two punch: chemo damages the cell’s defenses, and radiation delivers the final blow. This combo is standard for many cancers, including head, neck, and lung cancers.
Is radiation therapy only for advanced cancer?
No. Radiation is used at every stage. It can cure early-stage cancers on its own, shrink tumors before surgery, kill leftover cells after surgery, or ease symptoms in advanced cases. It’s one of the most flexible tools in cancer care.
What Comes Next
The future of radiation therapy isn’t just about better machines. It’s about smarter combinations. We’re moving toward treatments that don’t just destroy cancer cells but turn them into signals that wake up the immune system. With BRCA mutations as a roadmap, and immunotherapy as a partner, radiation is becoming a catalyst-not just a tool.For patients, this means more hope. For doctors, it means more precision. And for cancer as a whole, it means we’re finally learning how to fight it not just with force-but with biology.


Thomas Anderson
December 15, 2025 AT 14:56Radiation doesn't just blast cells-it messes with their DNA so bad they can't even reproduce right. It's wild how something so destructive can actually save lives.
My uncle went through it for prostate cancer, and now he's been clean for 5 years. No magic bullet, but this stuff works.
Alexis Wright
December 16, 2025 AT 12:31Let’s be real-radiation is just fancy nuclear terrorism wrapped in a white coat. They tell you it’s ‘targeted,’ but every time someone gets a second cancer from it, you know the system’s lying.
They don’t want you to know that the ‘precision’ is just marketing spin. The real goal? Profit. And patients? Disposable data points.
Daniel Wevik
December 16, 2025 AT 13:36The biological mechanisms described here are foundational to modern oncology. The induction of double-strand breaks via ionizing radiation triggers a cascade of DNA damage response pathways-ATM/ATR activation, γH2AX foci formation, and downstream p53-mediated cell cycle arrest.
What’s clinically significant is the differential repair efficiency between homologous recombination-proficient and deficient cells. BRCA-mutated tumors exhibit synthetic lethality with PARP inhibition, which synergizes with radiation-induced oxidative stress. This isn’t just therapy-it’s precision genomic warfare.
Tim Bartik
December 17, 2025 AT 12:52Y’all act like radiation is some kinda miracle cure but lemme tell ya-this whole thing is rigged by Big Pharma and the FDA.
They don’t want you to know that radiation can cause MORE cancer, and they cover it up so they can keep selling treatments. I heard a guy in Ohio who got radiation for throat cancer ended up with bone cancer in his jaw 3 years later. They told him it was ‘coincidence.’ LOL. Nothing’s a coincidence when the money’s flowing.
Rich Robertson
December 18, 2025 AT 00:47As someone who’s watched family members go through this, I’ve seen how radiation shifts from being feared to being respected.
It’s not just about killing cells-it’s about forcing the body to recognize cancer as an enemy. That immune activation part? That’s the real breakthrough. In India, where I’m from, many still think radiation is like a death sentence. But the truth? It’s giving people back years, sometimes decades.
It’s not perfect, but it’s one of the few tools that actually changes the game.
Natalie Koeber
December 18, 2025 AT 18:40Did you know the government secretly uses radiation therapy to implant microchips in patients? They call it ‘targeted treatment’ but it’s really a tracking system.
They use the DNA damage to embed nano-tech that connects to the 5G network. That’s why they say it’s ‘safe’-they don’t want you to know you’re being monitored through your own mutated cells.
And don’t even get me started on the flu shots-they’re the same tech.
Wade Mercer
December 20, 2025 AT 15:27It’s disturbing how casually people talk about zapping cells like it’s nothing. We’re playing God with biology and calling it science.
Every time someone gets radiation, a part of their body is permanently altered. No one talks about the emotional toll-the fear, the isolation, the feeling that your own cells are turning traitor.
Maybe we should ask if we’re healing-or just controlling.
Dwayne hiers
December 22, 2025 AT 06:50While the post accurately outlines the mechanistic basis of radiation-induced DNA damage, it underemphasizes the role of tumor microenvironment hypoxia in conferring radioresistance.
Hyperfractionated regimens and hypoxic cell sensitizers like nimorazole have demonstrated clinical efficacy in head and neck cancers. Additionally, the integration of AI-driven dosimetry reduces inter-operator variability by 37% in recent multicenter trials.
Emerging data on FLASH radiotherapy’s radiobiological sparing effect on normal tissue-mediated by reduced endothelial inflammation-is perhaps the most promising frontier.
Sarthak Jain
December 24, 2025 AT 00:00Man, I read this whole thing and I’m just blown away. I’m from India and we don’t have access to all this fancy tech, but my cousin got radiation for cervical cancer and it worked.
They used old-school machines, no AI, no FLASH-just good ol’ X-rays. But the part about BRCA and immune response? That’s wild. Even here, doctors are starting to talk about combining it with immunotherapy.
Hope this reaches more people. We need more awareness.