Understanding Meniere's Disease: What You Need to Know
If you’ve ever felt the room spin out of control or heard a sudden drop in your hearing, you might wonder if Meniere’s disease is behind it. This inner‑ear disorder can strike without warning, but knowing the basics helps you stay ahead. Below is a quick guide that breaks down the main signs, why they happen, and what you can actually do to feel better.
Common Signs and Triggers
People with Meniere’s typically notice three things: episodes of vertigo that last from minutes to hours, fluctuating hearing loss (often in one ear), and a feeling of fullness or pressure inside the ear. Some also pick up ringing (tinnitus) or a buzzing noise. The attacks don’t follow a set schedule – stress, salty foods, caffeine, or even changes in weather can bring them on.
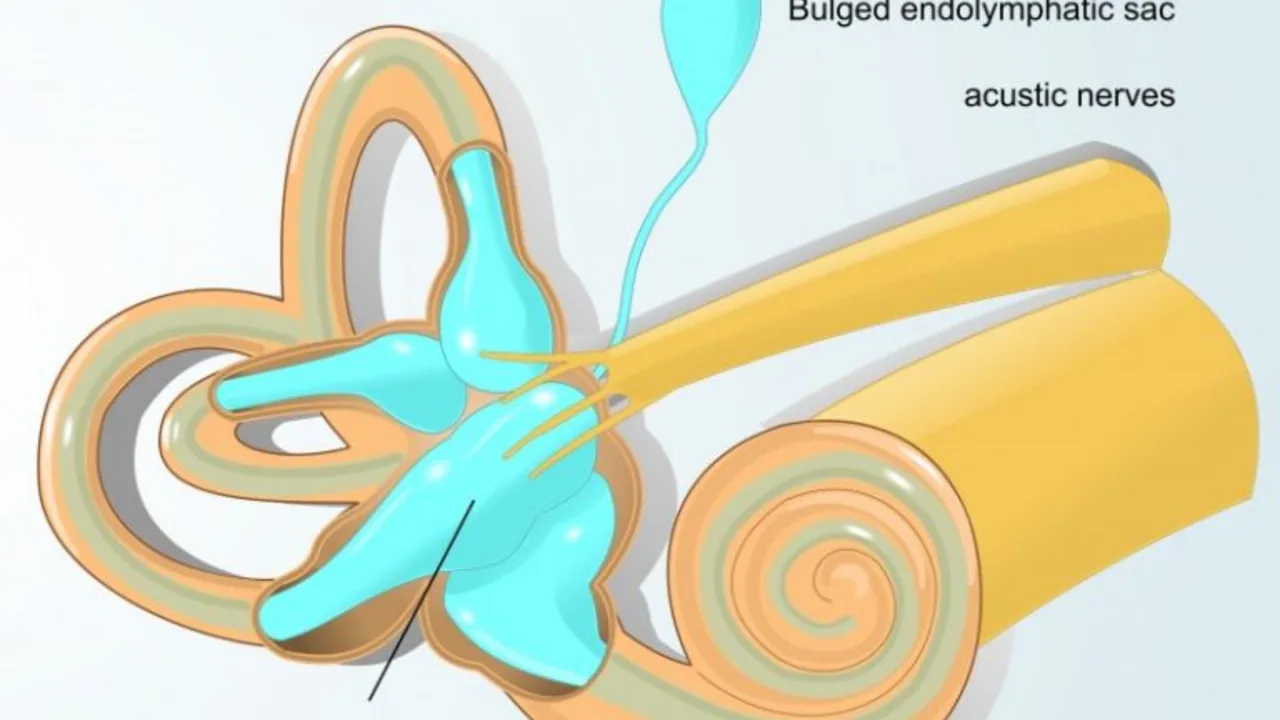
Why does it happen? The leading theory points to an excess of fluid, called endolymph, in the inner ear’s labyrinth. When that fluid builds up, it messes with the tiny hair cells that balance you and process sound. The result is the dizzy, muffled feeling you’ve probably experienced.
Managing the Condition
There’s no cure yet, but many strategies can cut down the frequency and severity of attacks. First, watch your salt intake. Cutting back to about 1,500 mg a day often eases fluid buildup. Staying hydrated with water (not sugary drinks) also helps the body regulate fluid balance.
Medication-wise, doctors may prescribe diuretics to drain excess fluid or anti‑nausea drugs for vertigo episodes. Some find relief with betahistine, a supplement that improves inner‑ear blood flow, though results vary.
Lifestyle tweaks matter too. Avoiding alcohol and caffeine during flare‑ups can keep symptoms from worsening. Gentle neck and head exercises, like slowly turning your head side‑to‑side, may improve circulation in the inner ear.
If attacks become frequent or your hearing drops sharply, a hearing aid or ear‑plug device can boost clarity. In severe cases, procedures such as a vestibular nerve section or gentamicin injections are options, but they’re usually a last resort.
Finally, stress management plays a big role. Techniques like deep‑breathing, short walks, or mindfulness can lower the hormone spikes that trigger fluid shifts. Keeping a simple diary—recording foods, stress levels, and attack timing—helps you spot patterns you can act on.
While Meniere’s disease can feel overwhelming, understanding the warning signs and making a few daily adjustments can dramatically improve your quality of life. If you suspect you have it, book an appointment with an ENT specialist or audiologist. Early diagnosis means you can start the right plan before the symptoms get out of hand.
Meniere's Disease and Vision: Understanding the Link
Hey there, beautiful souls! Today we're going to explore a unique topic, the connection between Meniere's Disease and vision problems. Often overlooked, this correlation is quite significant, increasing our understanding of how Meniere's Disease affects our day-to-day lives. We'll dive into the symptoms, causes, and ways to manage these visual disruptions caused by this condition. Stick with me, and let's reveal these insights together.