When a pharmacist hands you a pill bottle labeled NTI generics, they’re not just filling a prescription-they’re managing a high-stakes balancing act. These are drugs where a tiny change in dose or absorption can mean the difference between healing and harm. For medications like warfarin, levothyroxine, or phenytoin, even a 10% shift in blood levels can trigger a seizure, a stroke, or a dangerous blood clot. And yet, these same drugs are often swapped out for cheaper generic versions without a second thought. Pharmacists across the U.S. are sounding the alarm. They see the consequences firsthand: patients with unstable INR levels, thyroid levels that won’t stay in range, or seizures that didn’t happen before the switch.
What Makes a Drug an NTI Drug?
NTI stands for Narrow Therapeutic Index. It means the gap between a drug’s effective dose and its toxic dose is razor-thin. A standard drug like amoxicillin has a wide safety margin-you can take a little more or less without major consequences. But with NTI drugs, that margin is barely there. The FDA doesn’t publish an official list, but they flag certain drugs in the Orange Book with codes like ‘B’ to warn that substitution might not be safe. These include anticoagulants like warfarin, thyroid hormones like levothyroxine, anti-seizure meds like phenytoin and carbamazepine, and some immunosuppressants like cyclosporine.
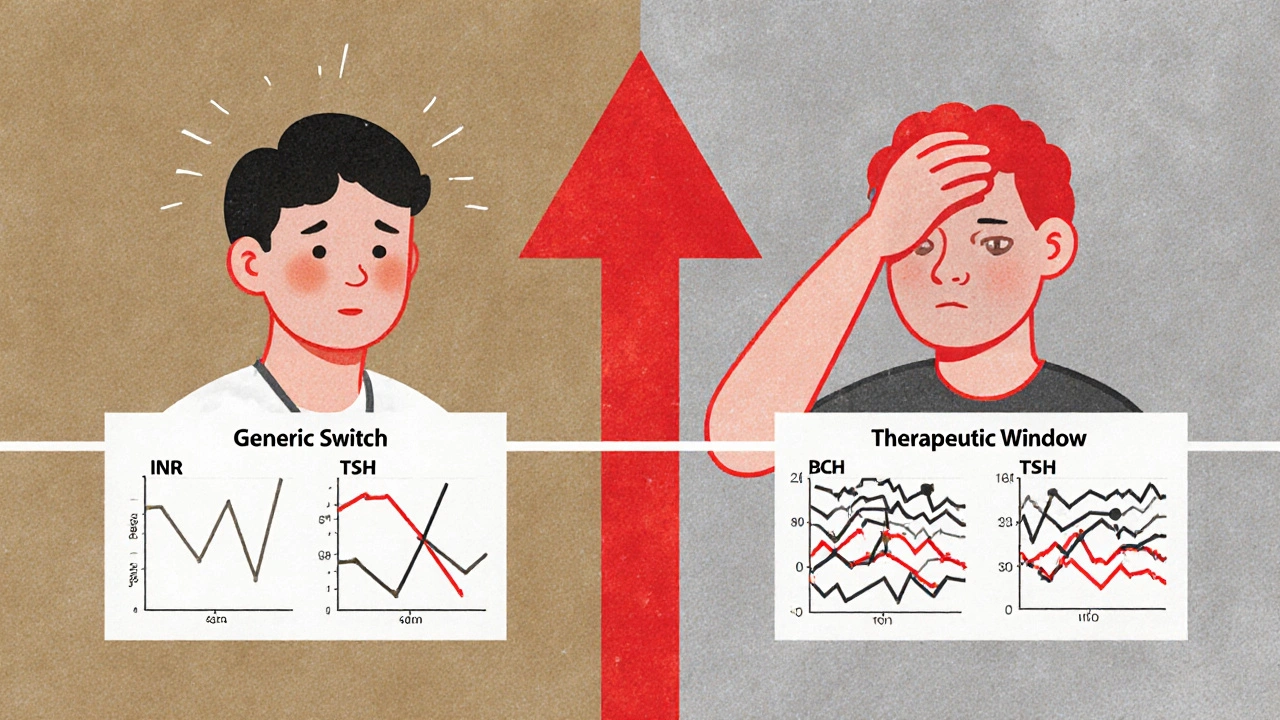
Here’s the catch: generic versions of these drugs are approved under the same rules as regular generics. For most drugs, bioequivalence is measured by how much of the drug enters the bloodstream-80% to 125% of the brand-name version is considered acceptable. But for NTI drugs, that range is too wide. The FDA recommends a tighter window: 90% to 111%. Only a handful of drugs actually get this stricter review. The rest? They’re approved under the same standards as ibuprofen or metformin. That’s a problem when a patient’s life depends on staying within 5% of the target concentration.
Why Pharmacists Are Worried
In 2024, the American Society of Health-System Pharmacists (ASHP) surveyed over 1,200 pharmacists. Two-thirds said they have real concerns about switching patients between different NTI generics. Why? Because the generics aren’t always the same. Even if two generics are labeled as the same drug-say, levothyroxine-they can come from different manufacturers with different fillers, coatings, or manufacturing processes. These differences don’t show up on a standard bioequivalence test, but they can change how the drug is absorbed.
One hospital pharmacist in Ohio reported three cases in six months where patients switched from one generic warfarin to another and ended up in the ER with dangerously high INR levels. Another in Florida saw a patient’s phenytoin levels drop 40% after switching to a new generic-leading to a seizure. These aren’t rare. The FDA’s adverse event database recorded 1,247 incidents linked to NTI generic switches between 2020 and 2024. That’s more than triple the number for non-NTI generics.
And it’s not just about the drug itself. It’s about consistency. If a patient gets one generic this month, then a different one next month, their body never gets a chance to stabilize. The FDA found that 23% of NTI drug shortages are worsened by constant switching between manufacturers. Pharmacists end up playing guesswork: Which version is this? Did the patient take the same one last month? Is this the one that worked, or the one that caused trouble?
The Cost-Saving Trap
It’s easy to see why NTI generics are pushed. They cost 80% to 85% less than brand-name versions. For a patient on levothyroxine, that’s $20 a month instead of $120. That’s huge for someone on a fixed income. But here’s what gets overlooked: the hidden costs. When a patient’s INR goes out of range, they need urgent blood tests, ER visits, maybe even hospitalization. A single warfarin-related adverse event can cost over $10,000 in emergency care. The savings from the generic? Gone.
And it’s not just money. It’s trust. Patients start to wonder: Why does my medication feel different? Why am I so tired now? Why did my doctor change my dose again? When pharmacists have to explain that the pill looks different but is supposed to work the same, it erodes confidence in the whole system. One community pharmacist in Texas told a patient, “I wouldn’t switch my own mother to a different generic warfarin.” That’s not an outlier-it’s a common sentiment among those who see the outcomes daily.
State Laws Are a Patchwork
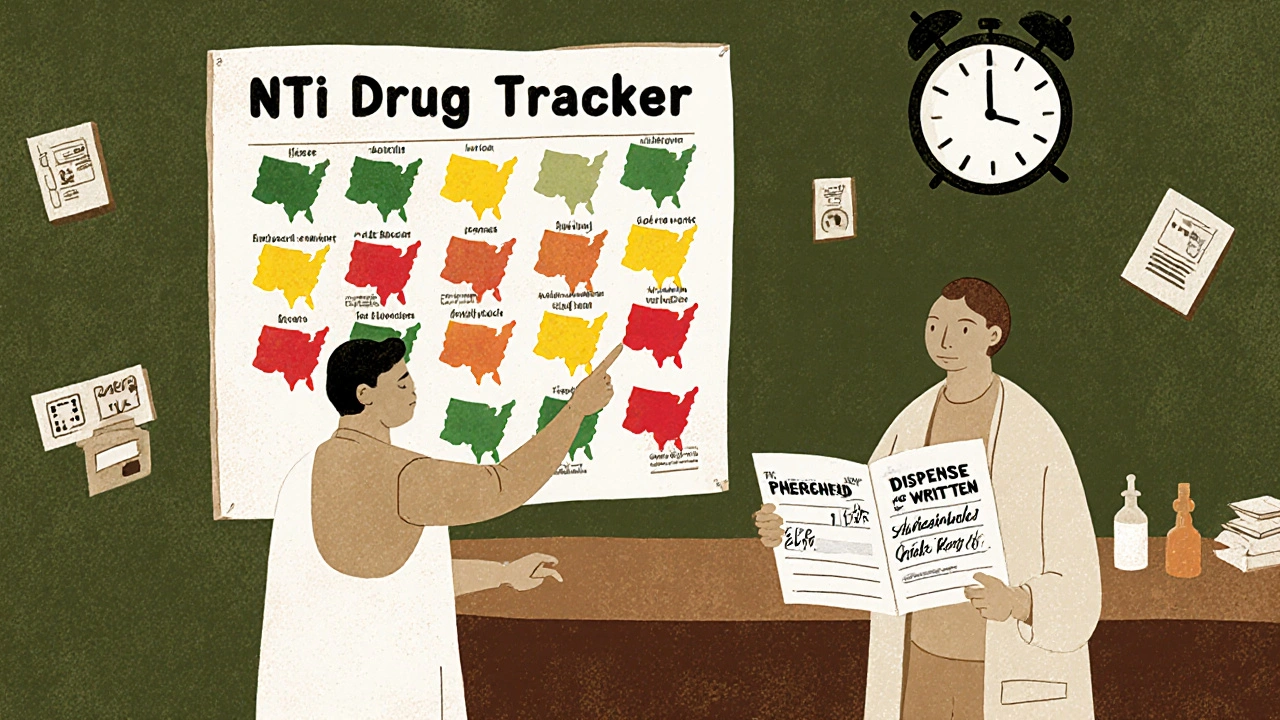
There’s no national rule for NTI drug substitution. As of January 2025, only 28 states have laws that restrict automatic substitution for NTI drugs. In some places, pharmacists can switch the drug without telling the prescriber. In others, they need a written note from the doctor. Six states outright ban automatic substitution for certain NTI drugs. That means a patient in California might get the same generic for a year, but if they move to Texas, they could get a different one-and no one tells their doctor.
And prescribers? Many don’t know the difference. A 2024 survey found that 42% of primary care doctors couldn’t name a single NTI drug. They just see “generic” on the script and assume it’s safe. That’s where pharmacists become the last line of defense. But they’re not always allowed to intervene. In states without protective laws, pharmacists are legally required to substitute unless the doctor writes “dispense as written.” That puts them in an impossible spot: follow the law, or protect the patient.
What Pharmacists Are Doing About It
Despite the challenges, many pharmacies are taking matters into their own hands. Hospitals with strong pharmacy departments now use a “single-source” policy: they pick one generic manufacturer for each NTI drug and stick with it. If a patient starts on that version, they stay on it. That’s working. A 2024 study showed a 58% drop in therapeutic instability when hospitals used this approach.
Some pharmacies now require patients to sign a consent form before switching NTI generics. Others use color-coded labels or electronic alerts in their systems to flag NTI drugs. Pharmacists are also pushing for better training. Eighty-one percent of pharmacy residency programs now include NTI drug management as a required module-something that wasn’t common five years ago.
And they’re using tools. The FDA’s Therapeutic Equivalence Ratings database is updated every quarter. The American Association of Managed Care Pharmacists (AMCP) and the Association for Accessible Medicines (AAM) both offer free NTI drug guides that list which drugs have stricter bioequivalence requirements. Pharmacists are using these to make smarter decisions, even when the law doesn’t require it.
What’s Changing in 2025 and Beyond
The FDA announced a new bioequivalence framework in April 2025, targeting 12 high-risk NTI drugs with stricter testing standards by 2026. This includes better methods for measuring drugs with complex chemistry-like those with multiple active isomers. It’s a step forward, but it’s slow. Only 12 out of the 42 drugs with known risks are on the list.
Meanwhile, Medicare’s new drug price negotiation program is including three NTI drugs-levothyroxine, warfarin, and phenytoin-in its first round. That’s good for cost control, but it’s risky. The program delays reimbursement by 21 days. For community pharmacies, that means they might not get paid for weeks after dispensing a high-cost NTI drug. Some are already warning they may stop stocking these drugs altogether. That’s not a theoretical problem-it’s happening in rural areas where pharmacies are already struggling to stay open.
Looking ahead, 74% of healthcare systems plan to create pharmacist-led NTI drug stewardship programs by 2027. That means pharmacists won’t just be dispensing-they’ll be monitoring, educating, and coordinating care. It’s a shift from passive filling to active management. And for NTI drugs, that’s exactly what patients need.
What Patients Should Know
If you’re on an NTI drug, here’s what you can do:
- Ask your pharmacist: “Is this the same brand and manufacturer as last time?”
- Don’t assume “generic” means identical. Even the same drug from two different companies can behave differently.
- If you feel different after a switch-fatigued, dizzy, anxious, or having new symptoms-tell your doctor and pharmacist immediately.
- Ask your doctor to write “dispense as written” or “do not substitute” on your prescription if you’ve had a bad reaction to a switch.
- Keep a log of your lab results (like INR for warfarin or TSH for levothyroxine) and bring them to every visit.
It’s not about rejecting generics. It’s about making sure the right drug is used at the right time. For NTI drugs, consistency isn’t a luxury-it’s a lifeline.
What does NTI mean in pharmacy?
NTI stands for Narrow Therapeutic Index. It means the difference between a drug’s effective dose and its toxic dose is very small. Even tiny changes in how the drug is absorbed can cause serious side effects or treatment failure. Examples include warfarin, levothyroxine, and phenytoin.
Can pharmacists substitute NTI generics without permission?
It depends on the state. In 28 states, pharmacists can substitute NTI generics without telling the prescriber. In six states, automatic substitution is banned. In others, the prescriber must write "dispense as written" to prevent substitution. Many pharmacists avoid switching NTI drugs even when allowed, due to safety concerns.
Why are NTI generics more dangerous than other generics?
Standard generics must be 80-125% as effective as the brand-name drug. For NTI drugs, that range is too wide. A 10% drop in absorption can make a life-saving drug ineffective. A 10% increase can cause toxicity. The FDA recommends a tighter 90-111% range for NTI drugs, but most aren’t held to that standard.
Which NTI drugs are most commonly switched?
The top three are warfarin (blood thinner), levothyroxine (thyroid hormone), and phenytoin (anti-seizure). Carbamazepine, cyclosporine, and digoxin are also frequently flagged. These drugs have well-documented cases of therapeutic instability after generic switches.
How can I tell if my generic NTI drug was switched?
Check the label for the manufacturer name and pill imprint. If it’s different from your last refill, it’s a new version. Ask your pharmacist: "Is this the same manufacturer as before?" If you notice new symptoms-like unusual fatigue, dizziness, or changes in lab results-ask whether a switch occurred.
Final Thoughts
NTI generics aren’t inherently bad. They save money. They make treatment accessible. But treating them like any other generic is dangerous. The system was built for drugs where precision doesn’t matter. These drugs demand more. They need consistent sourcing, clear communication, and pharmacists who are empowered to speak up. Until the rules catch up with the science, the burden falls on the people who know the drugs best-the pharmacists. And right now, they’re doing more than filling prescriptions. They’re preventing crises one pill at a time.






Chris Taylor
November 29, 2025 AT 06:33I’ve seen this happen with my grandma. She was on levothyroxine for years, then one day the pharmacy switched her to a different generic. She started feeling like she was walking through wet concrete-exhausted, foggy, no energy. Took three blood tests and a panic visit to the endo to figure out why. She’s back on the same brand now, and I swear, she’s a different person. These aren’t just pills. They’re lifelines.
Melissa Michaels
November 30, 2025 AT 02:49NTI drugs require precision. The current FDA bioequivalence standards for these medications are outdated and dangerously lax. A 20% variability window is acceptable for antibiotics but catastrophic for anticoagulants. The system must evolve to reflect clinical reality, not just regulatory convenience. Pharmacists are the last line of defense-and they’re overworked and under-supported.
Nathan Brown
December 1, 2025 AT 22:46It’s funny how we treat medicine like a commodity. We want cheap, we want fast, we want interchangeable. But when your life depends on a molecule being absorbed just right, you’re not buying laundry detergent. You’re trusting your biology to a factory in Ohio or India or wherever. That’s not capitalism. That’s Russian roulette with a prescription pad. I don’t know how we got here, but I know we’re not going to fix it by yelling at pharmacists.
Matthew Stanford
December 1, 2025 AT 23:42Single-source policies work. Hospitals that lock in one generic manufacturer for NTI drugs see way fewer adverse events. Simple. Effective. Why isn’t this standard everywhere? Because paperwork and profit win over patient safety. We need policy change, not just awareness.
Olivia Currie
December 2, 2025 AT 20:45OMG I JUST HAD A PANIC ATTACK READING THIS. My cousin had a seizure after switching warfarin generics. Like… what even IS our healthcare system?!? They’re playing Jenga with people’s lives and calling it ‘cost savings’ 😭😭😭
Curtis Ryan
December 4, 2025 AT 12:17so i was on phenytoin for like 5 years and they switched my generic and i had a seizure and then i was like wtf? and my dr was like oh yeah we switched to the cheaper one lol. like bro. i dont care if it saves 5 cents. i need to not die. 🤦♂️
Rajiv Vyas
December 4, 2025 AT 22:27NTI drugs? More like NTI lies. The FDA is in bed with Big Pharma. They don’t want you to know that the same drug from two different companies can kill you. They just want you to shut up and take the cheap pill. And guess what? The real manufacturers? They’re all owned by the same 3 corporations anyway. You’re being played.
farhiya jama
December 6, 2025 AT 13:52ugh another post about how pharmacists are heroes. yeah sure. but what about the 10 million people who just can’t afford brand name? do they just die? because that’s what this sounds like. ‘oh we can’t switch generics’-great, now my mom can’t pay rent. thanks for the moral superiority.
Astro Service
December 6, 2025 AT 22:58Why are we letting foreign companies make our medicine? This is why America is weak. If we made our own pills here, none of this would happen. China and India are poisoning our people with cheap generics. Ban imports. Make it in the USA. Patriotism saves lives.
DENIS GOLD
December 7, 2025 AT 13:15Oh wow. So pharmacists are superheroes now? Next you’ll tell me nurses are angels and doctors are saints. Meanwhile, the guy who wrote this post probably gets paid 200k a year to tell us how dangerous generics are. Meanwhile, my kid needs insulin. You want me to pay $120 a month for something that costs $3 to make? Go f*** yourself.
Ifeoma Ezeokoli
December 8, 2025 AT 19:02This reminds me of my cousin in Lagos-he got a new batch of antiepileptic drugs and had a seizure. Same story. Same problem. Global health is broken. We treat pills like widgets. But bodies? Bodies don’t care about supply chains. They just react. And sometimes, they break.
Daniel Rod
December 10, 2025 AT 06:29Just want to say thank you to every pharmacist who’s ever paused, looked at a script, and said ‘hold on.’ You’re the quiet guardians of human biology. 🙏💙 I’ve seen you argue with insurance companies, explain bioequivalence to confused patients, and stay late because someone’s INR was off by 0.5. You don’t get trophies. But you save lives. Every day.
gina rodriguez
December 11, 2025 AT 10:34My mom’s on levothyroxine and I made sure her doctor wrote ‘dispense as written’ after she had a bad reaction. It’s a small thing, but it made all the difference. If you’re on an NTI drug, just ask. Don’t be shy. Your pharmacist wants to help-you just have to ask them to.
Sue Barnes
December 12, 2025 AT 09:33People who don’t understand pharmacology shouldn’t be allowed to have opinions. This is basic science. If you can’t grasp that 80-125% is too wide for warfarin, you shouldn’t be reading medical posts. Go watch a YouTube video about how to tie your shoes instead.
jobin joshua
December 13, 2025 AT 21:27Bro I just got my warfarin from CVS and the pill looks different. I took a pic and posted it on TikTok. Now I got 12k likes and 3 pharmacists DM’d me. We’re gonna start a movement. #NTIisntanicknamed