What Exactly Is a Rotator Cuff Tear?
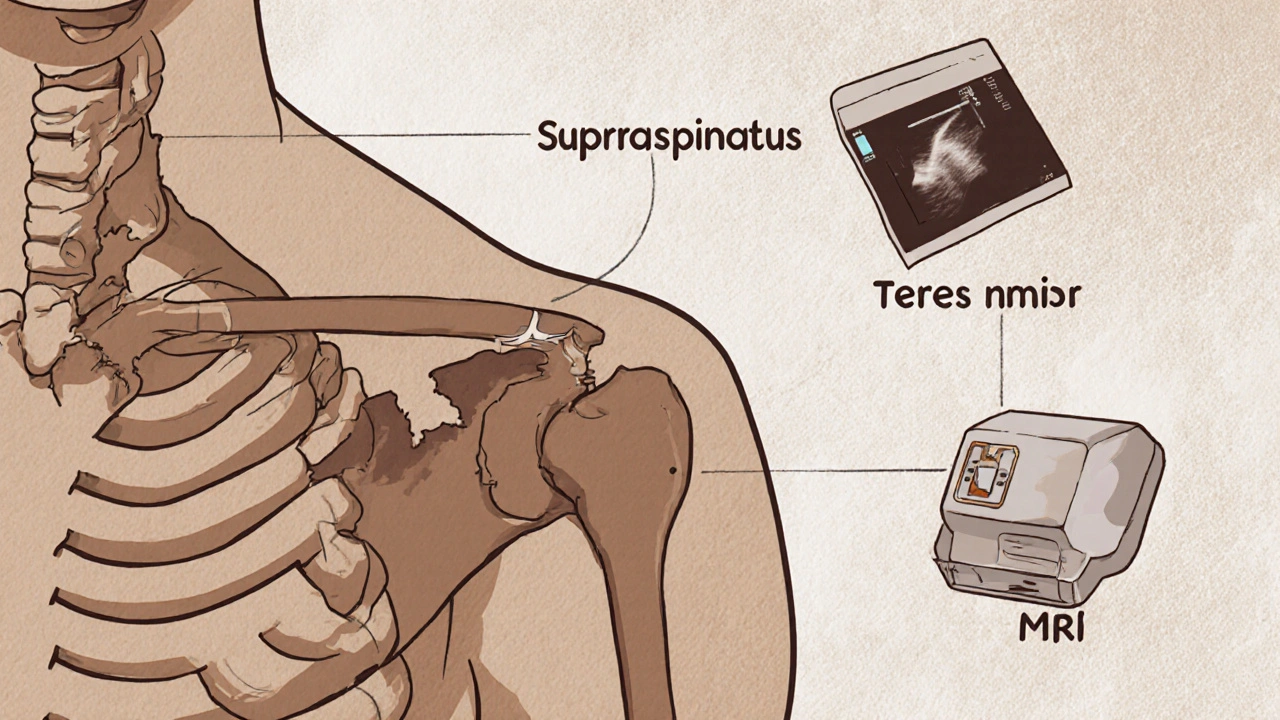
A rotator cuff tear happens when one or more of the four tendons that hold your shoulder joint together get damaged. These tendons connect the muscles of your shoulder blade to the top of your arm bone. The most commonly torn tendon is the supraspinatus, but the infraspinatus, teres minor, and subscapularis can also be affected. You don’t need a major accident to cause this. Over time, wear and tear, repetitive motions, or even just aging can lead to a tear. In fact, studies show that over half of people over 60 have a rotator cuff tear without ever having pain or symptoms. That’s right - you can have a tear and not know it.
How Do You Know If You Have One?
Most people notice a dull ache deep in the shoulder that gets worse when lifting the arm, reaching behind the back, or lying on that side at night. Weakness is another big sign - like struggling to lift a coffee cup or comb your hair. Doctors use simple physical tests to check for these signs. The Empty Can test (raising your arm straight out to the side with thumbs down) often triggers pain if the supraspinatus is torn. The Neer impingement test and Hawkins-Kennedy test press on the tendons to see if they catch or hurt. These aren’t just guesses - they’re proven methods backed by clinical guidelines from places like NewYork-Presbyterian.
Imaging: X-Rays, Ultrasound, and MRI - What’s the Difference?
Before jumping to scans, your doctor will start with an X-ray. It doesn’t show tendons, but it rules out bone problems like arthritis or bone spurs that could be causing similar pain. About 100% of initial cases use X-rays for this reason.
For the actual tendon damage, you’ve got two main choices: ultrasound and MRI. Ultrasound is cheaper - usually $200 to $400 - and faster. It lets the technician watch the tendon move in real time as you lift your arm. It’s also safe for people with metal implants, unlike MRI. A skilled sonographer can catch 87% to 91% of full-thickness tears. The catch? Only about 45% of general radiologists are trained well enough to do it accurately. If the tech isn’t experienced, the results can be misleading.
MRI gives a much clearer picture. It shows the exact size, location, and type of tear - whether it’s partial or full-thickness. It’s 92% accurate for full-thickness tears and up to 95% specific for partial ones. But it costs more - $500 to $1,200 - and takes longer. You also can’t move during the scan. For complex cases, surgical planning, or if ultrasound results are unclear, MRI is the gold standard. Most experts agree: start with ultrasound if it’s available from a qualified provider. Go straight to MRI if you’re young, active, or planning surgery.
When Is Surgery Necessary?
Not every tear needs surgery. In fact, the American Academy of Orthopaedic Surgeons now recommends trying physical therapy first for 6 to 8 weeks, even if imaging shows a tear. Why? Because many people get better without surgery. Studies show 85% of people with partial-thickness tears recover fully with rehab alone.
Surgery becomes the better option if:
- You’re under 65 and active - your job or hobbies demand shoulder strength
- You have a full-thickness tear larger than 1 cm
- Conservative treatment hasn’t helped after 3 months
- You lost significant strength suddenly - like after a fall
Today, over 90% of rotator cuff repairs are done arthroscopically. That means small incisions, a tiny camera, and specialized tools. It’s less invasive than the old open surgery. Recovery is faster, complications are lower (7.2% vs. 10.3% for open), and you can get back to daily tasks about 25% sooner.
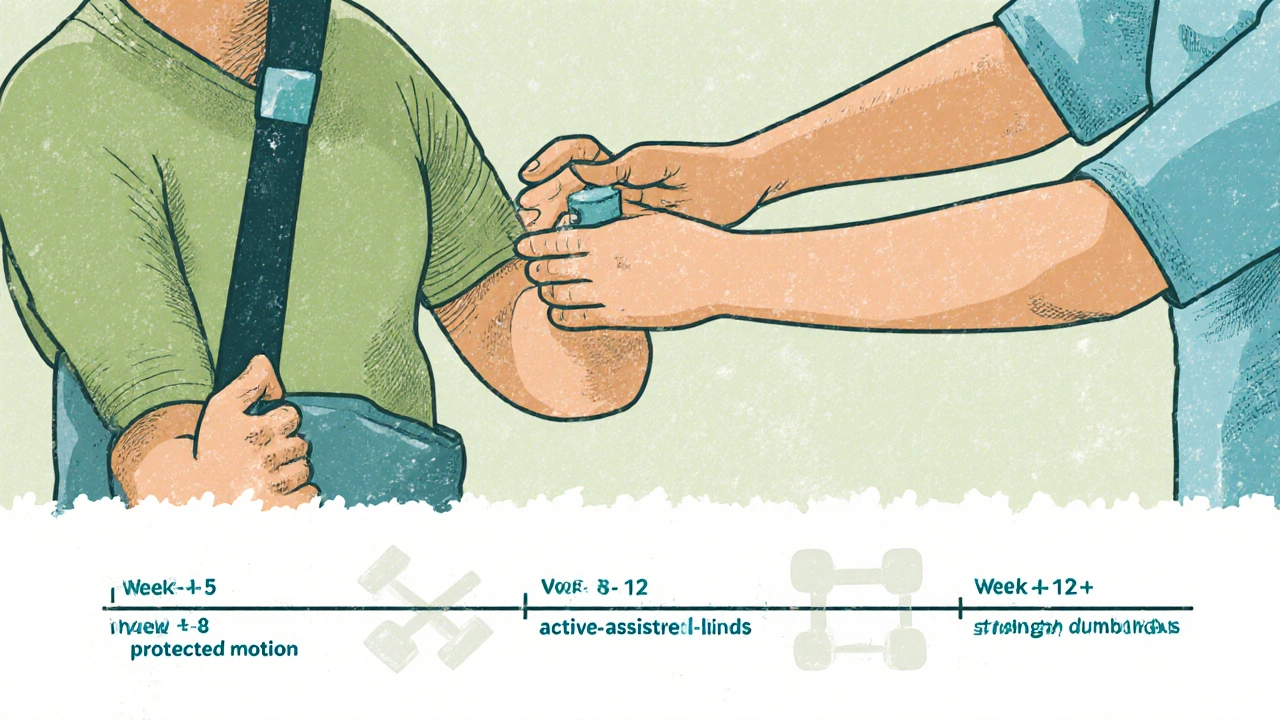
What Does Rotator Cuff Rehab Look Like?
Rehab isn’t one-size-fits-all. It’s broken into phases, and timing matters. Pushing too hard too soon can retear the tendon. Waiting too long can cause stiffness and muscle wasting.
Phase 1: Weeks 1-6 (Protection)
You’re in a sling for a short time, but movement starts early. Passive range-of-motion exercises - where someone else moves your arm for you - begin within days after surgery. No lifting. No pushing. Just gentle motion to prevent stiffness. This is critical. In the 1990s, people were immobilized for 6 weeks. Now, we know early motion leads to better outcomes.
Phase 2: Weeks 6-12 (Motion and Activation)
You start moving your arm on your own. Active-assisted exercises with resistance bands or light weights begin. The goal is to rebuild control without overloading the healing tendon. Pain is a guide - if it hurts during or after, you’re pushing too hard.
Phase 3: After Week 12 (Strength and Return)
Now you focus on strengthening the rotator cuff and surrounding muscles. Exercises like external rotation with bands, scapular squeezes, and eventually light dumbbell work. Most people return to normal activities by 4 to 6 months. Athletes may need 6 to 9 months before returning to sports.
Consistency beats intensity. Do your rehab exercises every day, even if it’s just 10 minutes. Skipping days slows progress. Studies show patients who stick to their rehab plan are twice as likely to have good long-term results.
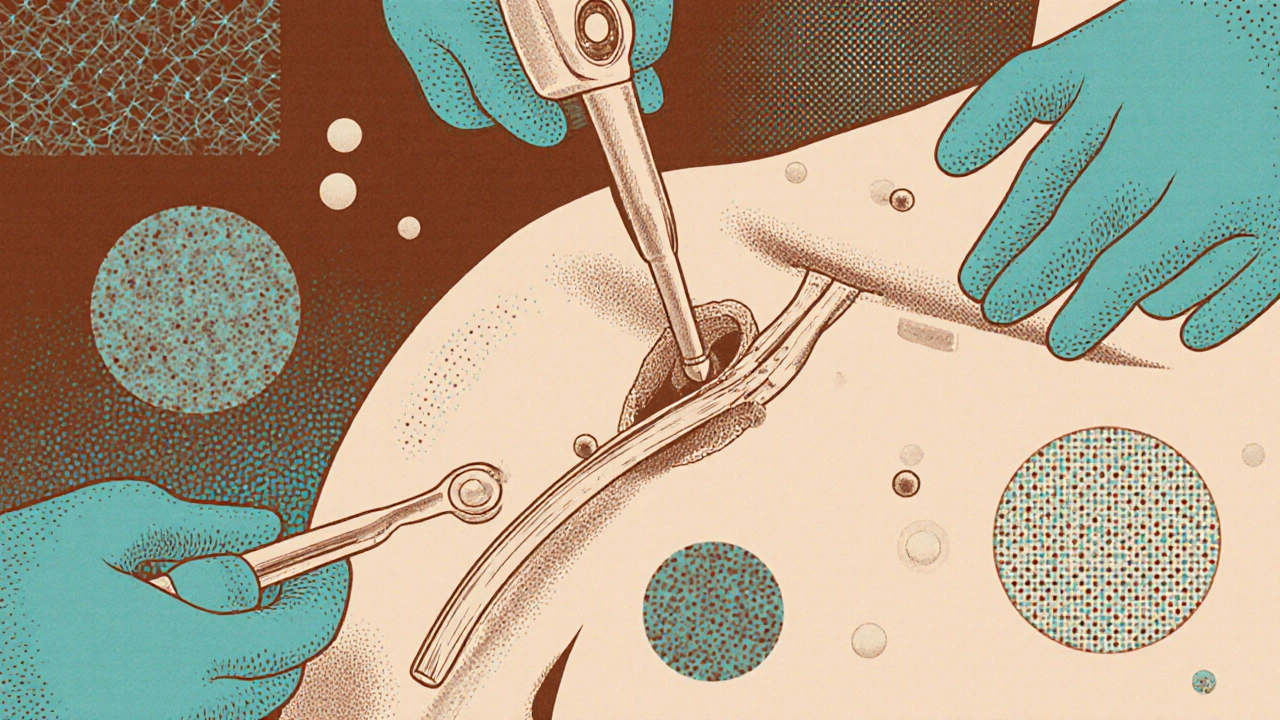
Surgical Options and What to Expect
Arthroscopic repair is the standard. Surgeons use tiny anchors to reattach the tendon to the bone. In some cases, especially with massive tears, they might use a patch to reinforce the repair. These patches are made from biological materials that help the tendon heal stronger.
Platelet-rich plasma (PRP) injections are sometimes used during surgery. The idea is that concentrated growth factors from your own blood help healing. But the evidence is mixed. A 2021 Cochrane Review found only moderate support for PRP. It’s not a magic fix. Don’t expect miracles.
Recovery after surgery isn’t easy. You’ll be sore. Your shoulder will feel stiff. But the pain usually drops off after the first 2 weeks. Most people report 82% satisfaction at the 5-year mark. But retear rates are real - 27% for large tears over 3 cm, compared to 12% for small ones under 1 cm. That’s why rehab and avoiding heavy lifting early on are non-negotiable.
What’s New in Rotator Cuff Care?
Technology is changing how we see and treat these injuries. Researchers are now using machine learning to analyze MRI scans. A 2023 study in Radiology: Artificial Intelligence showed AI could classify tear types with 89% accuracy - almost matching expert radiologists. This could mean faster, more consistent diagnoses in the future.
Another shift is in how we think about aging. Just because you’re over 60 doesn’t mean surgery is the only answer. Many older adults do well with rehab, even with a full-thickness tear. The key is function, not the scan. If you can lift your arm to wash your hair and sleep without pain, you might not need surgery at all.
What Happens If You Ignore It?
Leaving a tear untreated doesn’t always mean it gets worse. Some stay the same. But others can progress. The tendon can shrink, the muscle can turn to fat, and the shoulder joint can become unstable. Once that happens, repair becomes harder - and outcomes worse. That’s why early diagnosis and a clear plan matter.
Frequently Asked Questions
Can a rotator cuff tear heal without surgery?
Yes, many can - especially partial-thickness tears and in people over 60 who aren’t highly active. About 85% of patients with partial tears recover with physical therapy alone. Even some full-thickness tears stabilize over time if you avoid heavy lifting and follow a structured rehab program. The goal isn’t always to make the tear disappear - it’s to restore function and reduce pain.
Is MRI always needed for a rotator cuff tear?
No. Many doctors now start with ultrasound because it’s cheaper, faster, and just as accurate for full-thickness tears. MRI is reserved for complex cases, surgical planning, or when ultrasound results are unclear. The American Roentgen Ray Society recommends ultrasound as the first imaging test for suspected rotator cuff issues, unless there’s a strong reason to go straight to MRI.
How long does recovery take after rotator cuff surgery?
Most people return to light daily activities within 4 to 6 months. Full recovery - including returning to sports or heavy lifting - can take 6 to 9 months. The first 6 weeks are about protecting the repair. Strength builds slowly after that. Rushing the process increases the risk of retear. Patience is part of the treatment.
Can I prevent a rotator cuff tear?
You can’t stop aging, but you can reduce your risk. Strengthening the rotator cuff and shoulder blade muscles helps. Avoid repetitive overhead motions without rest. If you’re a swimmer, painter, or construction worker, take breaks and stretch regularly. Good posture also matters - slouching puts extra strain on the shoulder. Regular shoulder mobility work is one of the best preventative moves you can make.
Will I ever get my strength back after surgery?
Most people regain enough strength for daily life. Athletes and laborers may not get back to 100% of their pre-injury strength, especially with large or chronic tears. But function - being able to lift, reach, and sleep without pain - is usually restored. The key is sticking with rehab. Those who skip exercises or return to heavy work too soon often end up with weaker, less stable shoulders.
What’s Next?
If you’re dealing with shoulder pain, don’t assume it’s just “aging.” See a physiotherapist or sports doctor who understands rotator cuff injuries. Get a proper assessment - physical exam first, then imaging only if needed. Start rehab early. Avoid quick fixes like cortisone shots without a plan. And if surgery is recommended, make sure you understand why - and what your rehab plan looks like after.
The goal isn’t just to fix the tear. It’s to get you back to moving without pain - for good.


steve o'connor
November 24, 2025 AT 10:42Julie Pulvino
November 25, 2025 AT 14:25Melvina Zelee
November 26, 2025 AT 16:37Jessica Correa
November 26, 2025 AT 23:58james lucas
November 28, 2025 AT 22:12Miruna Alexandru
November 28, 2025 AT 23:56Justin Daniel
November 29, 2025 AT 06:32Shawn Daughhetee
November 30, 2025 AT 19:26Patrick Marsh
December 2, 2025 AT 11:11manish chaturvedi
December 4, 2025 AT 06:13Daniel Jean-Baptiste
December 5, 2025 AT 16:05ann smith
December 5, 2025 AT 20:30