Rhabdomyolysis Risk Calculator
Medication Interaction Risk Assessment
Enter your medications to check your risk of rhabdomyolysis from drug interactions. Based on FDA and European data.
Key Factors:
When you take a statin for cholesterol or colchicine for gout, you don’t expect your muscles to start breaking down. But when two medications mix in your body the wrong way, it can trigger a silent, dangerous process called rhabdomyolysis-a medical emergency where muscle cells die and spill their contents into your blood. This isn’t rare. It’s happening more often than most doctors and patients realize.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis means your skeletal muscles are breaking down rapidly. Inside those muscles are proteins like myoglobin, enzymes like creatine kinase (CK), and electrolytes like potassium. Normally, these stay locked inside muscle cells. But when the cell membrane gets damaged-by a drug interaction, trauma, or extreme exertion-they leak out. Myoglobin floods your kidneys. Potassium spikes in your blood. Your body can’t handle it.The classic signs are muscle pain, weakness, and dark urine-like cola or tea. But here’s the problem: about half of people with drug-induced rhabdomyolysis don’t have all three. Some just feel tired. Others get nausea, fever, or abdominal pain. By the time they notice dark urine, the damage may already be serious.
How Medications Cause This
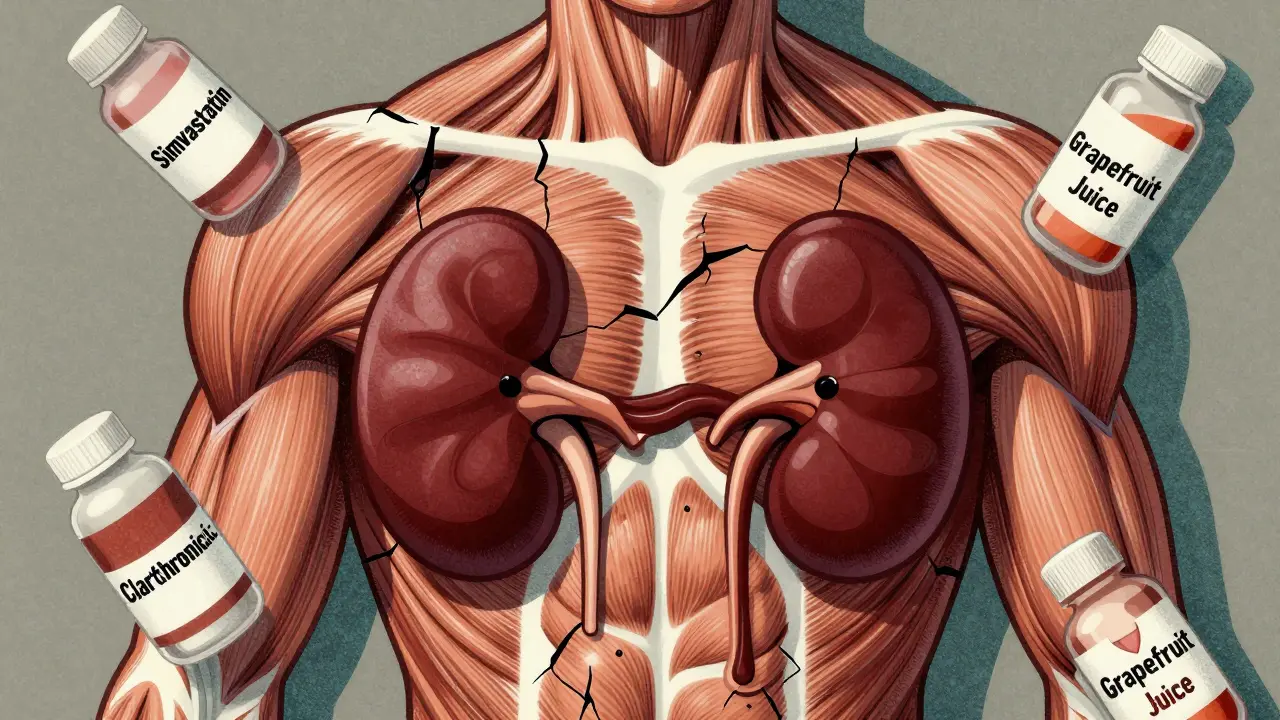
Not all drugs cause rhabdomyolysis on their own. It’s the combinations that are deadly. The biggest culprits? Statins-especially simvastatin and atorvastatin-when mixed with other medications that interfere with how your liver breaks them down.Your liver uses an enzyme called CYP3A4 to process many drugs. When something blocks that enzyme, statin levels skyrocket in your blood. That’s what happens with:
- Erythromycin (an antibiotic)
- Clarithromycin (another antibiotic)
- Itraconazole (an antifungal)
- Gemfibrozil (a cholesterol drug)
- Colchicine (for gout)
- Erlotinib (a cancer drug)
Take simvastatin with clarithromycin? Your risk jumps 18.7 times higher. Take colchicine with clarithromycin? Risk goes up 14 times. These aren’t theoretical numbers. They’re based on real hospital data from the FDA and European regulators.
Even common over-the-counter supplements like St. John’s Wort or grapefruit juice can interfere. Grapefruit blocks CYP3A4 too. One patient in Brisbane told me she drank grapefruit juice every morning with her simvastatin for years-until she woke up unable to stand, her urine dark as soy sauce. Her CK level was 48,000 U/L. Normal is under 200.
Who’s at Highest Risk?
It’s not just about what you take-it’s who you are.- Age 65+: Risk is 3.2 times higher. Older bodies clear drugs slower.
- Women: 1.7 times more likely than men to develop drug-induced rhabdomyolysis.
- People with kidney problems: If your eGFR is below 60, your risk jumps 4.5 times. Your kidneys can’t flush out the toxins.
- People on five or more medications: That’s 17.3 times higher risk. Polypharmacy isn’t just messy-it’s deadly.
And genetics play a role too. Some people carry a gene variant called SLCO1B1*5. If you’re of European descent, you’re 4.5 times more likely to get muscle damage from simvastatin-even at normal doses. Most doctors don’t test for this. They should.
When It Hits the Kidneys
The real danger isn’t the muscle pain. It’s what happens next. Myoglobin clogs the tiny tubes in your kidneys. Your kidneys shut down. Up to half of rhabdomyolysis patients develop acute kidney injury. Some need dialysis. About 5-15% die if this happens.That’s why doctors rush to give IV fluids-up to 3 liters in the first 6 hours. They also add sodium bicarbonate to make the urine less acidic. Myoglobin dissolves better in alkaline urine. It’s not fancy. It’s basic, life-saving physics.
But here’s the catch: if you wait until your urine turns dark, you’re already behind. CK levels above 5,000 U/L mean you’re in the danger zone. Above 10,000? You’re likely heading to the ICU. And if you’re on statins and start feeling unusually tired or achy after starting a new antibiotic? That’s not just a side effect. It’s a warning.
Real Cases, Real Consequences
A 71-year-old woman in Queensland was prescribed clarithromycin for a sinus infection. She’d been on colchicine for gout for years. Four days later, she couldn’t walk. Her urine was brown. Her CK was 28,500. She spent five days in hospital. Her kidneys recovered, but she still has muscle weakness two years later.A 58-year-old man with lung cancer was on erlotinib and simvastatin. His oncologist didn’t know about the interaction. Within 72 hours, his CK hit 42,000. He needed dialysis. He survived-but lost 40% of his muscle mass.
On Reddit’s r/Pharmacy, users report 68% of statin-related rhabdomyolysis cases involved a drug interaction-and 92% said their doctor never warned them. That’s not negligence. It’s ignorance. Most medical schools barely teach this.
What You Can Do
If you’re on any of these medications, here’s what to do:- Know your meds. Make a list. Include vitamins, supplements, and OTC drugs. Bring it to every appointment.
- Ask: “Could this interact with my other meds?” Especially if you’re on a statin. Don’t assume your pharmacist or doctor already checked.
- Watch for early signs. Unexplained muscle soreness, weakness, or dark urine? Don’t wait. Get a CK test.
- Get your kidney function checked if you’re over 65 or on multiple drugs. A simple eGFR test takes minutes.
- Never start a new antibiotic or antifungal without checking your statin. Even a short course can be dangerous.
And if you’re a caregiver for an elderly person? Pay attention. They might not complain about muscle pain. They might just say they’re “feeling off.” That could be the first sign.

The Bigger Picture
In the U.S., over 27,000 people are hospitalized each year for drug-induced rhabdomyolysis. Each case costs about $29,000. That’s $785 million a year-just for this one preventable condition.Regulators are catching on. The European Medicines Agency now requires statin labels to warn about CYP3A4 inhibitors. The FDA’s Sentinel system flagged a spike in cases after remdesivir was used for COVID-19. But hospitals still don’t have automated alerts for high-risk combinations.
Research is moving fast. Scientists are testing drugs that protect mitochondria-the energy factories in muscle cells-from statin damage. There’s even a $2.4 million NIH project to build real-time drug interaction alerts for doctors.
But until then, the responsibility falls on you. You’re the only one who knows what you’re taking. You’re the first to notice your body changing. Don’t wait for the system to protect you. Protect yourself.
Recovery and Long-Term Effects
Most people recover-if they get treated fast. But recovery isn’t quick. In non-kidney failure cases, it takes about 12 weeks to regain normal strength. If you needed dialysis? It can take over 6 months. And 44% of survivors still have muscle weakness at six months.Some never fully bounce back. Their muscles don’t regenerate the same way. They lose balance. They tire easily. They can’t climb stairs like they used to. That’s not just a side effect. That’s a life-altering consequence.
The good news? If caught early, rhabdomyolysis is treatable. The bad news? It’s often missed until it’s too late.
Can rhabdomyolysis happen from one medication, or only from interactions?
It can happen from one drug-like high-dose statins, especially in older adults or people with kidney disease. But most serious cases involve drug interactions. The biggest danger comes when two medications combine to overload your system. For example, a statin alone might cause muscle pain in 1 in 100 people. Add an antibiotic like clarithromycin, and that risk jumps to 1 in 5. Interactions are the silent killers.
How do I know if my muscle pain is serious?
Normal soreness from exercise fades in a day or two. Serious muscle pain from rhabdomyolysis is constant, deep, and doesn’t improve with rest. It often feels like you’ve been hit by a truck-even if you didn’t do anything strenuous. If you’re also feeling unusually tired, nauseous, or your urine is dark brown or red, treat it like an emergency. Call your doctor or go to the ER. A simple blood test for creatine kinase can confirm it in minutes.
Are all statins equally dangerous?
No. Simvastatin and lovastatin are the riskiest because they’re heavily processed by the CYP3A4 enzyme. Atorvastatin is less risky but still dangerous with certain drugs. Pravastatin and rosuvastatin are safer because they’re cleared differently-not through CYP3A4. If you’re on a statin and need a new medication, ask if you can switch to one of the safer ones.
Can I take statins again after having rhabdomyolysis?
It’s possible-but only under strict supervision. Most doctors avoid restarting statins entirely after a serious episode. If your cholesterol is still high, alternatives like ezetimibe or PCSK9 inhibitors may be safer. Never restart a statin on your own. If you do, you’re at high risk of another episode, often worse than the first.
Is there a blood test to check my risk before starting a statin?
Yes-the SLCO1B1 gene test can show if you’re genetically more likely to have muscle problems with simvastatin. But it’s not routine. Most doctors don’t order it unless you’ve had muscle symptoms before. If you’re over 65, on multiple meds, or have kidney issues, ask your doctor if this test makes sense for you. It costs under $200 and could prevent a life-threatening reaction.
What should I do if I’m on a statin and my doctor prescribes a new antibiotic?
Stop the statin until you’ve talked to your pharmacist or doctor. Ask: “Is this antibiotic safe with my statin?” If they’re unsure, ask for a different antibiotic. Don’t wait. Many people assume their doctor already checked the interaction. They didn’t. Over 90% of cases happen because no one asked the question.
Final Thoughts
Rhabdomyolysis from medication interactions isn’t a myth. It’s a real, preventable crisis. It’s not about being scared of pills-it’s about being smart with them. You’re not being paranoid if you ask about interactions. You’re being responsible.Every pill you take has a story. So does every muscle ache. Listen to your body. Ask the questions. Keep your meds list updated. And if something feels wrong-don’t wait. Your muscles, your kidneys, and your future self will thank you.