Every year, millions of people in the U.S. pay hundreds or even thousands of dollars more than they need to for prescription drugs-just because they don’t know a cheaper, equally effective option exists. Generic medications aren’t second-rate. They’re the exact same medicine, approved by the FDA, and often cost less than a cup of coffee. But how do you actually find out if your brand-name prescription has a generic version? It’s easier than you think, and it could save you hundreds-or even thousands-of dollars a year.
Why Generics Are Just as Good
Before you start searching, understand this: if a generic drug is approved by the FDA, it works the same way as the brand-name version. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration. That means if your doctor prescribed 10 mg of lisinopril, the generic version is also 10 mg of lisinopril. No differences in how it works in your body. The only difference? Price. In 2022, the average retail cost for a brand-name drug was $765.09. The same drug as a generic? Just $15.23. That’s not a typo. Generics save patients and the healthcare system billions every year. According to the FDA’s 2022 report, generics saved Americans $371 billion that year alone. But here’s the catch: not every drug has a generic. About 10% of medications still don’t, mostly because the brand-name maker still holds patent protection. Those patents usually last 17 years from filing, though extensions and legal maneuvers can delay generics for years. So you need to check.Ask Your Pharmacist First
The fastest, most reliable way to find out if a generic is available? Ask your pharmacist. Seriously. They see this every day. Pharmacists at CVS, Walgreens, Rite Aid, and Costco have real-time access to databases that track every approved generic alternative. In a 2022 JAMA Internal Medicine study, pharmacists correctly identified a generic alternative 98.7% of the time. When you pick up your prescription, say: "Is there a therapeutically equivalent generic available for this?" Don’t just ask, "Do you have a generic?" That’s too vague. You want to know if it’s approved as interchangeable. The key term here is "therapeutically equivalent." That’s what the FDA calls it. Most major pharmacies automatically offer generic substitution unless your doctor writes "dispense as written" or "no substitutions." But if you don’t ask, you might not even know a cheaper option was available.Use the FDA’s Drugs@FDA Database
If you want to check yourself, go straight to the source: the FDA’s Drugs@FDA website. It’s free, official, and updated daily. It lists every drug approved in the U.S., including over 14,000 generics. Here’s how to use it:- Go to Drugs@FDA.
- Type in the brand-name drug you’re taking (e.g., "Lipitor").
- Click on the brand-name result.
- Look for the "Therapeutic Equivalence Code" under "Approval History."
Check the Orange Book (Therapeutic Equivalence Ratings)
The FDA’s Approved Drug Products with Therapeutic Equivalence Evaluations-better known as the Orange Book-is the gold standard. It’s where all the ratings come from. You don’t need to read the whole thing. Just use the Drugs@FDA tool above. It pulls from the Orange Book automatically. But if you’re curious: the two-letter code tells you everything. The first letter: A = no known bioequivalence issues. B = potential issues. The second letter: A = single-source brand, B = multiple-source brand, X = not approved. AB = safe to substitute. BX = not recommended. If you see a "B" rating, talk to your doctor. It doesn’t mean the generic doesn’t work-it just means the FDA isn’t 100% confident it works the same way in everyone.Use GoodRx or Other Price Comparators
Sites like GoodRx, SingleCare, and RxSaver aren’t official FDA sources, but they’re great for price comparisons. They show you how much generics cost at different pharmacies near you. GoodRx is used by over 35 million Americans monthly. But here’s the limitation: they don’t tell you if a generic is therapeutically equivalent. They just show you prices. So if you see a $3 generic for your blood pressure pill, great. But if it’s not rated "AB," you might want to double-check with your doctor before switching.Check Your Medicare or Insurance Plan
If you’re on Medicare Part D, your plan’s formulary determines which generics they cover-and at what cost. Starting January 1, 2024, Medicare plans are required to show you real-time generic substitution info through the Medicare Plan Finder. Log in, enter your current medications, and see which ones have generics covered. Some plans even require you to use the generic-or you’ll pay more. Others have step therapy: you have to try the generic first before they’ll approve the brand. Don’t assume your plan automatically switches you. In 2023, a study found that 41% of Medicare beneficiaries didn’t know their plan had switched their medication. Always review your explanation of benefits.Watch Out for Common Pitfalls
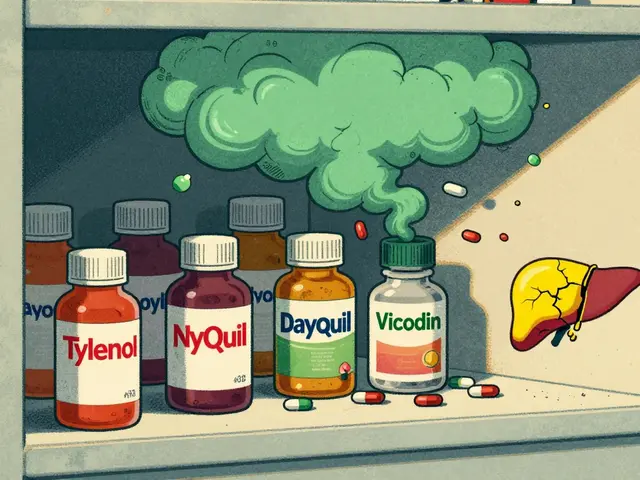
Not all generics are created equal. Some drugs are tricky:- Narrow therapeutic index drugs-like warfarin, levothyroxine, or phenytoin-require close monitoring. Even small changes in absorption can cause problems. Your doctor might prefer you stick with one brand or generic.
- Complex delivery systems-like inhalers, nasal sprays, or topical creams-can be harder to match exactly. The FDA’s approval standards are still evolving here.
- Similar-sounding names-like Zyrtec (cetirizine) and Zyprexa (olanzapine)-can lead to dangerous mix-ups. Always double-check the active ingredient on the label.

What If There’s No Generic?
If your drug doesn’t have a generic yet, don’t give up. Ask your doctor if there’s another drug in the same class that does. For example, if your brand-name statin doesn’t have a generic, maybe another statin does. Or if you’re on a newer antidepressant, your doctor might switch you to an older one with a generic version that works just as well. Also, check the ASHP Drug Shortages database. Sometimes, a generic exists-but it’s out of stock. That’s different from not having one at all.What’s Changing in 2024 and Beyond
The landscape is shifting fast. In October 2023, the FDA launched a simplified "Generic Drug Search" tool inside Drugs@FDA, designed for everyday users. It’s easier to navigate. Over 200,000 people used it in the first month. By Q3 2024, Epic Systems-the EHR platform used by over 250 million patients-will start showing FDA therapeutic equivalence ratings directly in doctors’ prescription screens. That means your doctor might get a pop-up saying: "Generic available. Cost: $12." And by 2028, 73% of top-selling drugs will have generic versions. The big ones are coming: Humira, Enbrel, and other biologics are finally facing competition. Biosimilars aren’t exact generics, but they’re close-and they’ll bring prices down too.Bottom Line: Ask, Check, Save
You don’t need to be a pharmacist or a researcher to save money on your prescriptions. Just follow these three steps:- Ask your pharmacist: "Is there a therapeutically equivalent generic?"
- Check the FDA’s Drugs@FDA for the "AB" rating if you want to verify.
- Save-sometimes over $1,000 a year.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove they are bioequivalent-meaning they are absorbed into the body at the same rate and to the same extent. Over 90% of prescriptions in the U.S. are filled with generics, and they’re used by millions daily without safety issues. The only exceptions are drugs with narrow therapeutic indexes, where even small differences matter. Always talk to your doctor if you’re unsure.
Why do some generic drugs cost more than others?
Price differences between generics happen because of competition. When only one company makes a generic, it can charge more. When five or six companies make it, prices drop fast. Also, some generics are made in different countries, and manufacturing costs vary. Pharmacy location, insurance plans, and coupon programs like GoodRx also affect what you pay. Always compare prices at multiple pharmacies.
Can I switch from a brand-name drug to a generic without telling my doctor?
For most drugs, yes. Pharmacists are allowed to substitute an FDA-approved generic unless your doctor specifically says "dispense as written." But for drugs like warfarin, levothyroxine, or epilepsy medications, even small changes can affect your health. It’s always best to inform your doctor when switching-especially if you’ve had issues before. Some doctors prefer you stay on one version to avoid confusion.
What does an "AB" rating mean on the FDA’s Orange Book?
An "AB" rating means the generic drug is considered therapeutically equivalent to the brand-name drug. The "A" means it’s bioequivalent-absorbed the same way in the body. The "B" means it’s a multiple-source product (not the original brand). Together, "AB" means you can safely switch without affecting how the drug works. This is the gold standard for substitution.
What if my insurance won’t cover the generic?
If your insurance denies coverage for a generic, ask your pharmacist to submit a prior authorization request. Sometimes, the plan only covers the brand-name drug because of a contract with the manufacturer. Your doctor can write a letter explaining why the generic is appropriate. You can also ask for a 30-day trial of the generic to prove it works. Or use a discount card like GoodRx to pay cash-often cheaper than your copay.