It’s one of the most dangerous moments in recovery: you’ve taken a break from your medication-maybe because you felt better, got hospitalized, or went through detox-and now you’re ready to start again. You think, “I used to take this dose just fine.” But your body doesn’t remember. And that’s where the risk hides.
When you stop taking certain medications-even for just a few days-your body loses tolerance. That means the same dose that once felt normal can now be deadly. This isn’t rare. It happens often with opioids, benzodiazepines, and some antidepressants. In fact, overdose after restarting medication is one of the leading causes of death among people who’ve been in treatment or incarceration. The CDC says nearly 62% of fatal opioid overdoses happen within 72 hours of leaving a hospital, jail, or rehab center. Why? Because tolerance drops faster than people realize.
Why Your Body Can’t Handle Your Old Dose
Your body adapts. When you take a medication regularly, your brain and liver adjust to process it. You build tolerance. But when you stop, that adaptation fades. For opioids like oxycodone or methadone, tolerance can drop by half in just three to five days. For benzodiazepines like alprazolam or clonazepam, it’s even quicker. One week off, and your system is back to near-zero baseline.
Think of it like this: if you haven’t lifted weights in months, you don’t go back to your old max weight on day one. You start light. The same rule applies to your brain and nervous system. Restarting at your old dose is like trying to bench press your former max after a year off-except your life depends on it.
Real cases show how deadly this is. A man in Brisbane stopped his prescribed oxycodone after a hospital stay. He returned home, took his old 30mg tablet, and was found unconscious two hours later. His family didn’t know he’d stopped. His doctor didn’t warn him. He survived-but barely. His story isn’t unique. Reddit threads like r/opiates are full of similar posts: “Took my usual dose after 10 days off. Ended up in ER.” “Thought I could handle it. Was wrong.”
Which Medications Carry the Highest Risk?
Not all medications are equal when restarting. Some are far more dangerous than others. Here are the top three categories with the highest overdose risk after a break:
- Opioids (e.g., oxycodone, hydrocodone, methadone, fentanyl): These slow breathing. Even a small drop in tolerance can cause respiratory failure. Fentanyl is especially deadly because it’s 50-100 times stronger than morphine. A dose that was safe before can now kill.
- Benzodiazepines (e.g., diazepam, lorazepam, clonazepam): These are sedatives. Stopping them can cause rebound anxiety and seizures. Restarting too fast can lead to extreme drowsiness, confusion, or coma-especially if combined with alcohol or sleep aids.
- Antidepressants (MAOIs and SNRIs) (e.g., phenelzine, venlafaxine): Restarting these too soon after stopping can cause serotonin syndrome-a rare but life-threatening condition. Symptoms include high fever, rapid heart rate, confusion, and muscle rigidity. A 2016 case study showed serotonin toxicity after restarting venlafaxine just 10 days after stopping an MAOI.
Other medications like antipsychotics (quetiapine, olanzapine) can cause dangerous drops in blood pressure when restarted at old doses. That’s why the Medicines Learning Portal recommends starting at just 25% of the previous dose for quetiapine after a week off.
The Safe Restart Protocol: Start Low, Go Slow
There’s no one-size-fits-all rule, but medical experts agree on one principle: start low, go slow. Here’s how to do it right:
- Don’t restart alone. Always consult your doctor or pharmacist before restarting. If you were in treatment or jail, ask for a formal restart plan.
- Start at 25-50% of your old dose. For opioids, begin with a quarter of what you used to take. For benzodiazepines, start at 20-30%. For antidepressants, wait at least two weeks after stopping MAOIs before starting a new one.
- Wait 24-48 hours between dose increases. Don’t rush. Your body needs time to readjust. If you feel dizzy, overly sleepy, or have trouble breathing, stop and call your doctor.
- Monitor for warning signs. Key red flags: breathing fewer than 12 times per minute, pinpoint pupils (for opioids), extreme drowsiness, confusion, or inability to stay awake. These mean your body can’t handle the dose.
- Have naloxone on hand. If you’re restarting an opioid, get naloxone (Narcan). Keep it in your home. Teach someone close to you how to use it. Washington State’s guidelines say this isn’t optional-it’s lifesaving.
For methadone, the Washington State Department of Health recommends starting at 25% of the previous dose and never exceeding 30mg on day one. For buprenorphine, you may need to wait until withdrawal symptoms appear before restarting. Each medication has its own timeline.
What About Polypharmacy?
One of the most overlooked dangers is mixing medications. If you’re restarting an opioid, but you’re also taking sleeping pills, muscle relaxers, or alcohol-even a glass of wine-you’re multiplying the risk. These substances all depress the central nervous system. Together, they can shut down breathing faster than any single drug.
Studies show that 70% of fatal overdoses after restart involve more than one sedating substance. The Calgary Clinical Pharmacology service says: “Never assume a combination is safe just because you used to take it.” If you’re on more than one medication, ask your pharmacist to run a drug interaction check. Tools like Medscape or Micromedex can flag dangerous combinations.
When to Wait Longer
Some medications need more than a few days to restart safely:
- MAOIs (monoamine oxidase inhibitors): Wait at least 14 days before starting any SSRI, SNRI, or even certain painkillers like tramadol. Serotonin syndrome can strike quickly and hard.
- Long-acting opioids (methadone, extended-release oxycodone): Tolerance drops slower than with short-acting drugs, but restarting too fast still causes overdose. Wait 7-10 days before restarting, and start at 25%.
- Antidepressants (paroxetine, fluoxetine): These linger in your system for weeks. Restarting too soon can cause buildup. Wait until plasma levels drop-usually 2-4 weeks-before restarting at low doses.
There’s no rush. The goal isn’t to get back to your old dose fast. It’s to get back safely. Rushing = risk. Patience = survival.
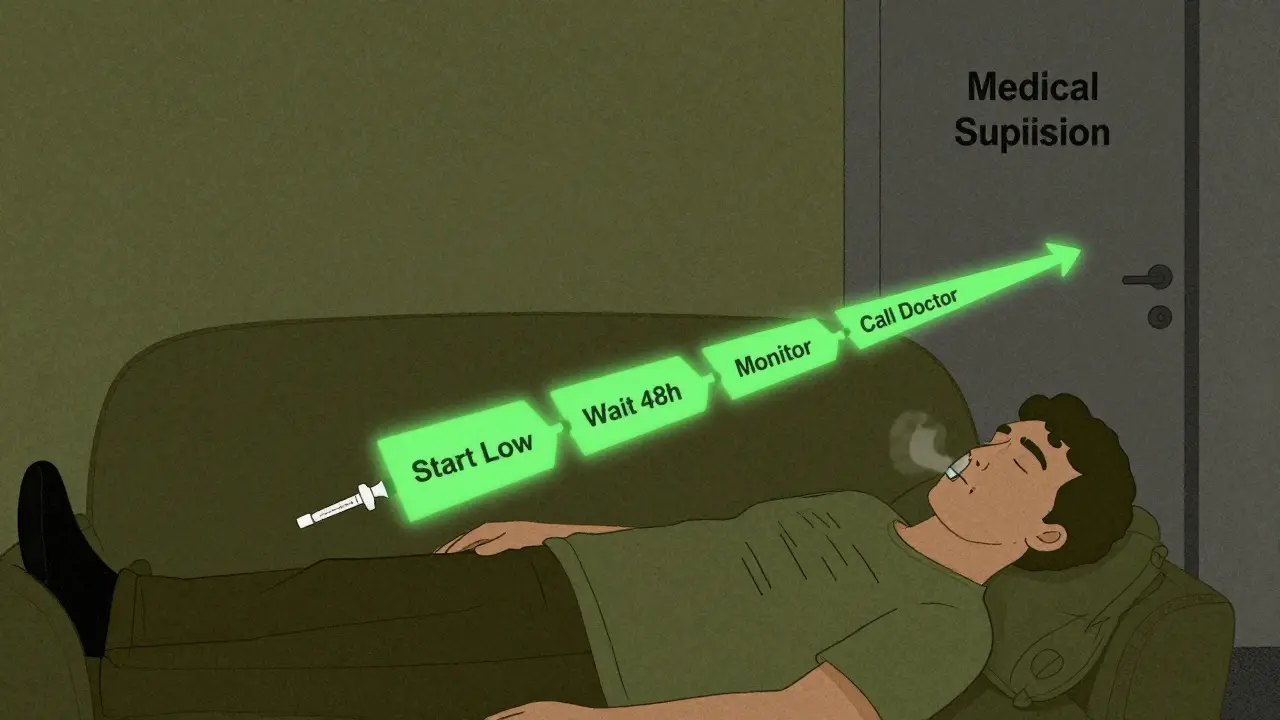
Medical Supervision Isn’t Optional
Trying to restart on your own is like driving blindfolded. You might get lucky-but you’re playing Russian roulette with your life.
Research from Evoke Wellness shows that patients who restart under medical supervision have an 87% success rate. Those who don’t? Only 42%. Why? Because professionals can monitor vital signs, adjust doses in real time, and catch early signs of trouble.
Hospitals in urban areas have formal restart protocols. But in rural areas, only 32% do. If you’re in a rural area, don’t wait. Call your local pharmacy. Ask if they offer supervised restart programs. Some community health centers now offer free, one-time consultations for this exact issue.
And if you’re coming out of jail or prison? You’re at the highest risk. The CDC says overdose risk spikes 40-fold in the first two weeks after release. That’s why programs like the Opioid Response Network now train correctional staff to hand out naloxone and restart instructions before release.
What’s New in 2026?
Things are changing. In February 2024, the American Society of Addiction Medicine rolled out a new 10-point scoring system to help doctors calculate safe restart doses based on your abstinence length, past dose, liver function, and other health factors. It’s not perfect-but it’s a step forward.
Also, Johns Hopkins published a study in April 2023 showing that giving extended-release naltrexone (Vivitrol) before restarting opioids cuts overdose risk by 73% in the first 30 days. It’s not widely available yet, but it’s being tested in Australia and the U.S.
And soon, wearable devices might automatically detect dangerous breathing patterns and inject naloxone before you lose consciousness. OpiSafe Technologies is in Phase 3 trials. This tech could save thousands.
But none of that matters if you don’t take action now.
Key Takeaways
- Overdose after restarting medication is common-and preventable.
- Your body loses tolerance fast. Even a week off can make your old dose deadly.
- Always restart under medical supervision. Never guess.
- Start at 25-50% of your previous dose. Increase slowly.
- Keep naloxone on hand if restarting opioids.
- Avoid alcohol, sleep aids, and benzodiazepines during restart.
Can I restart my medication the same day I stop it?
No. Even if you feel fine, your body’s tolerance drops within hours. Restarting immediately risks overdose. Always wait at least 24-48 hours, and consult a doctor before restarting any medication.
Is it safe to restart opioids after a month off?
Yes-but you must start at a much lower dose. After a month, your tolerance is nearly gone. Even if you used to take 80mg of oxycodone daily, you should start at 10-20mg, and increase only after 24-48 hours with no side effects. Never assume your old dose is still safe.
What if I don’t have a doctor to ask?
Call your local pharmacy. Pharmacists are trained to advise on medication restarts. Many offer free consultations. In Australia, you can also contact the Alcohol and Drug Foundation (ADF) for free support. They’ll connect you with a healthcare provider who can help.
Can I use naloxone if I’m not sure I overdosed?
Yes. Naloxone is safe to use even if you’re not sure. It only works on opioids and has no effect on other drugs. If someone is unresponsive, breathing slowly, or has blue lips, give naloxone. It can’t hurt them-it might save their life.
How long does it take to rebuild tolerance?
It varies. For opioids, tolerance rebuilds over days to weeks, depending on the drug and dose. But you should never try to rebuild it by increasing your dose quickly. That’s how overdoses happen. Work with a provider to find the lowest effective dose-then stay there.





