For people struggling with type 2 diabetes and extra weight, the old choices felt limited: take pills that barely moved the needle on blood sugar, or inject insulin and gain more weight. That’s changed. GLP-1 receptor agonists aren’t just another diabetes drug-they’re rewriting the rules for metabolic health. These medications don’t just lower A1C; they help you lose significant weight, reduce cravings, and even protect your heart. And it’s not magic. It’s science-your body’s own signals, amplified.
How GLP-1 Agonists Work: More Than Just a Shot
GLP-1 is a hormone your gut makes after you eat. It tells your pancreas to release insulin only when blood sugar is high-no guessing, no crashes. It also slows down your stomach so food doesn’t spike your sugar. And it talks to your brain: you’re full. GLP-1 receptor agonists mimic this natural hormone. They’re synthetic versions that stick around longer, turning up the volume on your body’s own weight and blood sugar controls.
Think of it like this: your body already has a system to manage food and glucose. These drugs just help that system work better. They don’t force insulin out regardless of need. They don’t flood your system. They guide it. That’s why they rarely cause low blood sugar on their own.
Weight Loss That Actually Sticks-For a While
The weight loss numbers are hard to ignore. In clinical trials, semaglutide (Wegovy) helped people lose an average of 15% of their body weight over a year. That’s not a few pounds. That’s someone who weighed 220 pounds dropping to 187. In the STEP 8 trial, people on semaglutide lost nearly twice as much weight as those on liraglutide (Saxenda). Tirzepatide (Zepbound), a newer dual-agonist, pushed that even further-20% weight loss on average.
But here’s what patients really notice: the hunger fades. You don’t feel like you’re starving. You stop craving chips, cookies, soda. One user on Reddit said, “I looked at a donut and felt nothing. It wasn’t willpower. It was like my brain forgot how to want it.” That’s not coincidence. GLP-1 agonists act on the hypothalamus-the brain’s appetite control center-quieting hunger signals and boosting fullness signals. It’s not suppressing appetite. It’s resetting it.
A1C Reduction: Clear, Consistent, and Powerful
For blood sugar, GLP-1 agonists are among the most effective tools available. Semaglutide (Ozempic) at 1.0 mg weekly lowered A1C by 1.8% on average in the SUSTAIN 1 trial. That’s a drop from 8.7% to 6.9%-moving from poorly controlled to well-controlled diabetes in one go. Liraglutide (Victoza) brought A1C down by 1.14%. Compare that to metformin, which typically lowers A1C by 0.5-1.0%, or sulfonylureas, which can cause weight gain and hypoglycemia.
What makes this powerful is the dual win: better A1C without the weight gain you get from insulin or older pills. For someone with obesity and diabetes, that’s rare. Most diabetes meds make weight harder to manage. These make it easier.
How They Stack Up Against Other Drugs
Let’s be clear: not all diabetes drugs are equal when it comes to weight.
- Sulfonylureas (e.g., glimepiride): Lower A1C but cause 2-4 kg weight gain.
- Insulin: Effective for sugar control but leads to 4-10 kg weight gain on average.
- DPP-4 inhibitors (e.g., sitagliptin): Mild A1C drop (0.5-1.0%), almost no weight change.
- SGLT2 inhibitors (e.g., empagliflozin): Lose 2-5 kg, good for heart and kidneys, but work differently-by making you pee out sugar.
- GLP-1 agonists: Lose 5-15% body weight, drop A1C by 1.0-1.8%, no hypoglycemia risk alone.
The difference isn’t just in the numbers-it’s in the experience. You’re not just managing diabetes. You’re reversing metabolic stress.
Side Effects: Real, But Manageable
Let’s not sugarcoat it: nausea, vomiting, and diarrhea happen. About 30-50% of people experience gastrointestinal issues, especially when starting or increasing the dose. The good news? They usually fade within weeks. Most patients tolerate them well after the first 8-12 weeks.
Here’s how to make it easier:
- Start low. The first dose of semaglutide is only 0.25 mg per week.
- Go slow. Dose increases happen monthly, not weekly.
- Eat smaller, lower-fat meals during titration. High-fat foods worsen nausea.
- Take the shot at night. Some find sleeping through the worst of the side effects helps.
- Use OTC meds like dimenhydrinate (Dramamine) if nausea is strong.
Needle anxiety? Common. But most people get comfortable after 2-3 tries. The pens are designed to be simple-no visible needle, quiet release. Over 85% of users master it after training.
The Big Catch: It’s Not a Cure
Here’s what no one tells you upfront: when you stop, the weight comes back. Studies show people regain 50-70% of lost weight within a year after stopping GLP-1 agonists. That’s not failure-it’s biology. Your body fights to return to its old weight set point. The drug didn’t change your metabolism permanently. It just gave you a better control system while you were on it.
This means: if you want to keep the results, you likely need to stay on the medication. For many, that’s a long-term commitment-not a quick fix. It’s like blood pressure medicine. You don’t stop when your pressure normalizes. You keep taking it because the condition doesn’t go away.
Cost and Access: The Real Barrier
In the U.S., without insurance, a monthly supply of Wegovy or Ozempic can cost $1,000-$1,200. That’s out of reach for most. Even with insurance, prior authorization is common. Medicare Part D covers about 62% of prescriptions, but often only after you’ve tried and failed other weight loss methods.
And there’s a shortage. Since early 2022, semaglutide has been on the FDA’s shortage list due to overwhelming demand. Some pharmacies can’t keep it in stock. This isn’t just a pricing issue-it’s a systemic bottleneck.

What’s Next? The Future of GLP-1 Drugs
The next wave is even more exciting. Tirzepatide (Zepbound) combines GLP-1 with GIP, another gut hormone. It’s showing even better weight loss and A1C results. Oral versions of semaglutide are now approved for diabetes (Rybelsus), and trials for an oral weight-loss version are underway.
Researchers are also testing these drugs for fatty liver disease, heart failure, and even Alzheimer’s. Early data from The Lancet showed semaglutide reduced liver fat by 52% in 48 weeks. The STEP-HFpEF trial found improved exercise tolerance in heart failure patients with obesity.
But there are open questions. Long-term safety beyond 5-7 years? Effects on mental health? Impact on fertility? These are still being studied. Experts agree: the benefits so far outweigh risks-but we’re still learning.
Who Benefits Most?
These drugs aren’t for everyone. They’re FDA-approved for:
- Type 2 diabetes (Ozempic, Mounjaro, Trulicity)
- Obesity (BMI ≥30) or overweight with weight-related conditions (BMI ≥27) - Wegovy, Zepbound, Saxenda
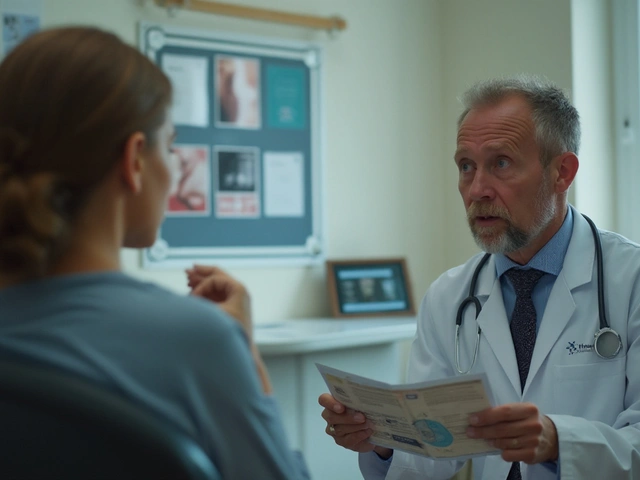
If you have type 2 diabetes and are overweight, you’re a strong candidate. If you have prediabetes and are trying to prevent progression, they may help-but aren’t yet approved for that. Insurance usually requires documented attempts at diet and exercise first.
They’re not a substitute for lifestyle. They’re a tool to make lifestyle easier. People who combine them with movement and balanced eating see the best, most lasting results.
Do GLP-1 agonists cause low blood sugar?
Not on their own. GLP-1 agonists only stimulate insulin when blood sugar is high, so they rarely cause hypoglycemia. But if you’re also taking insulin or sulfonylureas, your risk goes up. Always talk to your doctor about adjusting other meds if you start a GLP-1 agonist.
How long does it take to see results?
You might notice less hunger and smaller portions within days. Weight loss usually starts after 4-8 weeks. The full effect on A1C and weight takes 16-20 weeks. Most people reach their maximum weight loss around 68 weeks (about 16 months).
Can I drink alcohol while on a GLP-1 agonist?
Moderate alcohol is usually fine, but it can worsen nausea, especially early on. Alcohol also affects blood sugar, so if you’re diabetic, monitor closely. Many people find they naturally drink less because they don’t crave it as much.
Is it safe to use GLP-1 agonists long-term?
Current data shows they’re safe for at least 5-7 years. The LEADER trial with liraglutide showed a 13% reduction in heart attacks, strokes, and cardiovascular death in high-risk patients. Ongoing studies are tracking longer-term safety, especially for newer drugs like tirzepatide.
Are there any serious risks?
Rare but serious risks include pancreatitis, gallbladder disease, and a possible increased risk of thyroid tumors (seen in rodent studies, not confirmed in humans). If you have a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome, you should avoid these drugs. Always discuss your full medical history with your doctor.
What if I can’t afford it?
Some manufacturers offer patient assistance programs. Novo Nordisk has a savings card for Ozempic and Wegovy that can lower costs to $25 per month for eligible patients. Generic versions aren’t available yet, but oral semaglutide (Rybelsus) is cheaper than injectables and may be covered under different insurance tiers. Talk to your pharmacist or doctor about options.
Final Thought: A Tool, Not a Miracle
GLP-1 receptor agonists are the most powerful weight and blood sugar tools we’ve had in decades. They’re not perfect. They’re not cheap. They’re not a cure. But for the first time, we have a way to help people lose weight without starving, lower A1C without gaining pounds, and protect their heart along the way. If you’re struggling with diabetes and weight, they’re worth talking about-not because they’re magic, but because they’re real, and they work.





stephen riyo
November 25, 2025 AT 15:55Okay but like… why is everyone acting like this is the first time anyone’s ever lost weight without starving? I’ve been on metformin for 5 years and I still crave donuts. Now I’m supposed to believe some fancy shot just… turns off hunger? That’s not science-that’s a cult. I’ve seen people on these drugs look like ghosts. And then they stop? Boom. Back to 300 lbs. This isn’t a cure, it’s a Band-Aid with a $1,200 price tag.
Mqondisi Gumede
November 25, 2025 AT 23:27Let me tell you something about Western medicine you won’t hear in your pharma ads. You think your body needs a synthetic hormone to tell you you’re full? Your ancestors didn’t have Ozempic and they didn’t die of diabetes. They ate real food. They moved. They fasted. Now we’ve turned biology into a subscription service. This isn’t progress. It’s surrender. The real problem? You’ve forgotten how to listen to your own body. Not your doctor. Not your pen. YOU.
Douglas Fisher
November 26, 2025 AT 21:49I just want to say how much I appreciate how clear and thoughtful this post is. I’ve been on semaglutide for 8 months now, and honestly? The nausea was brutal at first-I thought I’d quit after week two. But I stuck with it, went slow, ate smaller meals, and now? I don’t even think about junk food. It’s not magic. It’s not willpower. It’s just… my brain stopped screaming for sugar. I lost 42 pounds. My A1C went from 8.9 to 5.7. And I didn’t have to count calories. That’s huge. Thank you for explaining the science so well.
Albert Guasch
November 27, 2025 AT 23:45It is imperative to recognize that GLP-1 receptor agonists represent a paradigmatic shift in the therapeutic architecture of metabolic syndrome management. Unlike conventional pharmacologic agents, which operate via exogenous insulin stimulation or renal glucosuria, these compounds modulate endogenous neuroendocrine signaling pathways with remarkable specificity. The clinical implications-namely, concomitant glycemic control and adiposity reduction without hypoglycemic risk-are unprecedented in the annals of endocrinology. One must, however, remain cognizant of the pharmacoeconomic constraints and the imperative for longitudinal safety surveillance.
Ginger Henderson
November 29, 2025 AT 21:43Wait, so I’m supposed to believe this is better than just eating less and moving more? Like… what? I’ve lost 30 lbs just by cutting soda and walking my dog. This feels like a scam to sell expensive pens.
Bethany Buckley
December 1, 2025 AT 06:59While the pharmacokinetics of GLP-1 agonists are undeniably elegant, the ontological implications are far more profound. We are witnessing the commodification of satiety-a neoliberal reconfiguration of biological need into a marketable state. The fact that we’ve normalized pharmaceutical intervention for hunger as a moral failing speaks volumes about our cultural pathology. 🤔🩺💸 Also, the packaging of these pens? Aesthetic genius. Zero needles. So… very… clean.
Jesús Vásquez pino
December 3, 2025 AT 01:32Look, I get it-these drugs work. I’ve seen it. My cousin lost 60 lbs on tirzepatide. But here’s the truth no one says: you’re not fixing the root cause. You’re just silencing the symptoms. And if you’re not eating clean, moving, and sleeping right? You’re just buying time. Also, if you’re not on this because you have diabetes or obesity? Stop. This isn’t for influencers who want a six-pack. It’s for people who are sick. Don’t turn medicine into a trend.
hannah mitchell
December 3, 2025 AT 03:16My mom’s on Ozempic. She’s 68. Used to be terrified of needles. Now she does it while watching her morning show. Said the hardest part was getting used to not feeling hungry all the time. She says it’s the first time in 30 years she’s felt like her body isn’t fighting her. I don’t know if it’s perfect. But it’s helped her. And that’s enough for now.