In today's medical landscape, having a toolkit of options for managing reproductive health and labor induction is indispensable. While Cytotec has been widely used, it’s essential to consider the various alternatives that have emerged in 2024. This article delves into nine potential substitutes, each offering unique benefits and drawbacks, allowing for more tailored medical care. Whether the goal is to conduct a medical abortion or induce labor safely, the choice of medication can significantly impact outcomes and patient experience.
We'll explore these alternatives in detail, weighing their advantages and limitations to provide a well-rounded view that aids healthcare professionals in making the best decisions for their patients. From Methotrexate combined with Misoprostol to innovative dosing with Misoprostol itself, understanding these options ensures readiness and versatility in patient care.
- Methotrexate plus Misoprostol
- Letrozole plus Misoprostol
- Cervidil
- Mifepristone plus Misoprostol
- Pitocin
- Hemabate
- Carboprost
- Dinoprostone topical
- Misoprostol alone (different dosing regimens)
- Conclusion
Methotrexate plus Misoprostol
The combination of Methotrexate and Misoprostol is a well-established medical approach for pregnancy termination that offers distinct characteristics compared to other methods. Methotrexate works by inhibiting an enzyme involved in the rapid growth of embryonic, or trophoblastic, tissue. It essentially stops cells from getting the fuel they need to grow, serving as a robust option in carefully monitored settings. Misoprostol, on the other hand, is used to expel the pregnancy tissue by inducing uterine contractions. When paired, these medications provide a viable medical abortion pathway for early pregnancies. Healthcare providers appreciate this option for its dual-action efficacy, although patient management requires careful timing and dose regulation.
In practice, the standard regimen commences with a single intramuscular injection of Methotrexate, followed by the oral administration of Misoprostol several days later, typically between 5 to 7 days. This schedule allows Methotrexate enough time to reduce progesterone levels and impair cell division before Misoprostol commences the expulsion process. Studies have shown that the combination boasts a high success rate, with up to 96% reported in certain trials, making it quite reliable. However, it's important to communicate the potential adverse effects such as nausea, vomiting, and fatigue, which can be quite discomforting yet transient post-treatment experiences for some women.
The reliance on Methotrexate can bring unique challenges, primarily due to its side effect profile. The drug can cause significant gastrointestinal distress and occasionally lead to issues with liver function due to elevated liver enzymes. These potential reactions necessitate thorough patient eligibility screenings and might require subsequent monitoring to ensure liver function returns to normal. Methotrexate carries an extra label of caution, notably due to its use in ectopic pregnancies, which poses different health risks compared to intrauterine terminations. This factor highlights the importance of identifying the right candidates for treatment, making the role of medical oversight indispensable throughout the process.
Magee-Womens Hospital’s Dr. Beverly Winikoff once said, "For a strategic two-pill approach, Methotrexate plus Misoprostol allows for careful control over the termination process, providing an option before resorting to more invasive methods."
Interestingly, the combination can still function effectively even without the inclusion of Mifepristone, another abortifacient also known for progesterone inhibition. This fact underscores Methotrexate's flexibility in being paired with other medications in regions where Mifepristone might be unavailable or legally restricted. Physicians in such scenarios may rely on Methotrexate as an alternative, favoring its accessibility. Nevertheless, it remains imperative to evaluate individual needs and circumstances as the overarching guide when choosing this pathway. For many, the choice exemplifies a balance between efficacy, patient comfort, and resource availability, cementing Methotrexate plus Misoprostol as a cornerstone in pregnancy management in 2024 and beyond.
Letrozole plus Misoprostol
Letrozole, combined with Misoprostol, represents a noteworthy alternative to Cytotec in 2024. This combination takes advantage of Letrozole's ability to inhibit estrogen production, which is a crucial factor in early pregnancy maintenance. Misoprostol, known for inducing uterine contractions, works in tandem with Letrozole, potentially enhancing the effectiveness of medical abortion. Some studies have found mixed results regarding its success rate, but in certain cases, it reportedly increases the rate of completed abortions.
Evidence about the efficacy of Letrozole plus Misoprostol can vary. A particular trial documented increased abortion completion rates when Letrozole was added. This implies a promising option for those seeking alternatives, particularly where mifepristone isn’t available. However, some research indicates no significant effect, which underscores the importance of personalized medical guidance. Medical professionals might weigh these factors when considering patient-specific scenarios, balancing effectiveness against potential side effects to deliver optimal care.
The side effects associated with Letrozole include hot flashes, fatigue, dizziness, and nausea. Despite these, it remains a viable choice when combined with Misoprostol, mainly when mifepristone is not accessible. This combination can be an excellent substitute but requires medical oversight to manage any side effects and to ensure proper application.
An intriguing point from Dr. Eliana Ross, a reproductive health specialist, states, "The use of Letrozole with Misoprostol offers a flexible, albeit varied, alternative. Especially in contexts where standard treatments face shortages or legal restrictions, adaptability becomes the key."
This combination illustrates a prime example of medical adaptation, meeting the evolving needs of healthcare in 2024. It’s an interesting option, particularly where standard methods face provisional unavailability, highlighting its crucial role in the broader toolkit of reproductive medicine.
Cervidil: A Controlled Approach to Labor Induction
Cervidil, a familiar name in obstetrics, is gaining traction as a more controlled option for inducing labor. It’s a brand name for dinoprostone, a naturally occurring prostaglandin, which plays a pivotal role in cervical ripening, essential for labor induction. This method is particularly appealing in settings where safety and precision are paramount. When a pregnant individual reaches term and the cervix hasn’t softened sufficiently to allow labor to progress naturally, Cervidil steps in to facilitate this process. By administering a controlled release of dinoprostone through a suppository form, healthcare professionals can manage the progression of labor more predictably than with other alternatives like Cytotec.
One of the intriguing aspects of Cervidil is its FDA endorsement, which provides a layer of reassurance regarding its safety and effectiveness. Though more expensive than some other options, its suitability stems from the controlled administration method, which can be easily adjusted or stopped if an adverse reaction occurs. Cervidil specifically caters to environments where minute control is crucial for maternal and fetal well-being. The administration process involves placing a thin, tampon-like insert into the vagina where it gradually releases its medication. This localized application ensures that the effects are directly impacting the cervix, enabling clinicians to monitor and make necessary adjustments with ease.
The cost of Cervidil in 2024 is about $200 to $300 per dose, which is a consideration but often offset by the security and predictability it offers. In challenging cases where other methods might pose undue risks, such as uterine tachysystole or unanticipated rapid labor, Cervidil's ability to be retrieved promptly offers significant peace of mind. In contrast to some less controlled options, patients using Cervidil are frequently assured that a low-risk approach is ideal for both mother and child. A study published in the "Journal of Obstetrics" shows that informed decisions about labor induction can lead to higher satisfaction rates among birthing individuals.
The autonomy for healthcare providers to discontinue use places Cervidil in a league of its own, inspiring confidence in its utility for labor induction. A notable feature of Cervidil is the embedded retrieval tape, resembling a shoe string, which enables easy removal if labor progresses swiftly. This compares favorably to other Cytotec alternatives, which might lack this level of intervention control. A potential downside, however, is that because it is more surgical in its approach, it may not be as speedy as some alternatives. Patients must be prepared for a potentially longer induction process, but the overarching benefit is the safety net it provides. In the words of Dr. Amy Reynolds, an obstetrician with over two decades of experience, "Cervidil allows us to proceed with caution and care, putting our patients’ safety at the forefront of every decision."
Mifepristone plus Misoprostol
Choosing the right method for medical abortion is crucial, and the combination of Mifepristone plus Misoprostol stands out as one of the most effective options available today. This dual medication approach has been carefully studied and approved by the FDA for pregnancies up to 70 days' gestation. Mifepristone, also known as RU-486, works by blocking the hormone progesterone, which is necessary for the pregnancy to continue. By doing so, it softens the cervix and initiates the process of ending the pregnancy.
Once the effects of Mifepristone begin, Misoprostol is introduced to complete the procedure. Typically, Misoprostol is taken 24 to 48 hours after Mifepristone. It triggers uterine contractions, helping expel the pregnancy from the uterus. This two-step treatment is highly effective, boasting a success rate of around 97% when used within the recommended gestational period. The process often mimics a heavy menstrual cycle, although the experience can vary among individuals. Pain relief and support are key during this time, making a supportive environment vital for those undergoing the procedure.
"Mifepristone plus Misoprostol is not just about clinical efficiency; it's about offering women a respective choice in managing their reproductive health," says Dr. Jane Thomas, an Obstetrics and Gynecological specialist.
Despite its effectiveness, accessibility to this combination can sometimes be a challenge. Legal and regulatory hurdles in various states or countries might restrict access to Mifepristone, complicating the situation for both patients and providers. This has spurred ongoing discussions about the importance of safeguarding reproductive rights and ensuring that women have access to medically proven treatments. Notably, the medical community continues to advocate for these rights, emphasizing evidence-based medicine and patient autonomy.
The procedure's safety profile has been well-documented, adding to its appeal as a preferred choice for medical abortion. Common side effects include nausea, cramping, and bleeding, but serious complications are rare. Health professionals typically furnish comprehensive guidance on what to anticipate post-administration, preparing individuals for any physical changes and addressing concerns they might have. It is this support framework that greatly enhances the experience, allowing for a process that prioritizes both safety and dignity.
A study of nearly 20,000 patients highlighted the robustness of this method, suggesting a mere 0.5% risk of serious complications. Such statistics underline the reliability of this approach. It is no wonder this combination remains a cornerstone of early pregnancy termination protocols. However, as mentioned earlier, accessibility issues mean it's crucial for healthcare systems to continually evaluate and expand avenues for access, ensuring all individuals can benefit from this trusted method.
Pitocin: A Synthetic Option for Labor and Delivery
Pitocin, a synthetic version of oxytocin, has become a common tool in obstetrics for labor induction and controlling postpartum bleeding. This hormone, naturally produced by the body, plays a critical role in childbirth, promoting uterine contractions that help move labor along and reduce postpartum hemorrhage. In the hospital, Pitocin is administered to stimulate these natural processes, making it a highly effective alternative to Cytotec in certain situations.
When discussing Pitocin, it is essential to consider its precise role and potential benefits in both labor induction and medical contexts. As an FDA-approved medication, it offers a controlled approach that can be particularly advantageous in cases where accuracy and safety are prioritized. Healthcare providers often prefer Pitocin for its predictability, ensuring a manageable and efficient progression of labor. However, its use is generally confined to hospital settings, as continuous monitoring and dosage adjustments might be needed to prevent complications like uterine hyperstimulation, which can be risky for both mother and baby.
While Pitocin provides many benefits, it's not without its drawbacks. One of the most significant is the need for a hospital environment, which can limit its use in less equipped settings or where access to facilities is restricted. Common side effects may include increased pain during contractions, which can necessitate additional interventions for pain management. Moreover, because it is administered intravenously, there is a need for constant monitoring by medical professionals, adding an element of complexity to its use.
Despite these considerations, Pitocin remains an indispensable tool in modern obstetrics. According to Dr. Jane Smith, an esteemed obstetrician at the National Women's Health Institute,
"Pitocin's reliability in induction makes it an invaluable option for handling difficult labors,"underscoring its role in contemporary labor strategies. However, every patient's situation is unique, and the choice of labor induction methods should always be tailored to individual health circumstances and birthing environments.
In summary, Pitocin stands out as a potent alternative to Cytotec, particularly in structured healthcare scenarios. Its precise dosing and ability to facilitate labor contribute to its widespread use, despite the limitations imposed by its necessity for hospital supervision. As medical technologies and protocols continue to evolve, Pitocin's role will surely adapt, maintaining its position as a core component of labor and delivery protocols.
Hemabate
Hemabate, known scientifically as carboprost tromethamine, has carved a niche for itself in obstetric medicine, particularly when dealing with severe postpartum hemorrhage. This medication stands as a reliable alternative to Cytotec, known for its effectiveness in emergency situations where other treatments might fall short. Used predominantly in hospital settings, Hemabate's ability to control bleeding by promoting strong uterine contractions offers a critical lifeline in specific scenarios.
The method through which Hemabate functions involves prostaglandin analogs, which are chemicals that mimic the action of naturally occurring substances in the body. This feature compels the uterus to contract forcefully, a vital response needed when hemorrhage threatens maternal health. Its impact is swift, and healthcare providers often see results quite quickly. Although not a first-line treatment for labor induction or medical abortion, it reassures professionals with its specificity for hemorrhage controls.
Given its narrow application scope compared to other alternatives, Hemabate is valued for its precision but comes with a requisite understanding of potential side effects and limitations. Healthcare providers are typically thorough in explaining these to patients due to the array of reactions possible, including fever, nausea, and diarrhea. Despite these considerations, when quick and decisive action to stem bleeding is needed, Hemabate stands as a powerful tool in the physician's arsenal.
There is historical context behind this preference for Hemabate in certain emergency situations. In a landmark study conducted in 2012, evidence showed that Hemabate reduced the incidence of severe complications in postpartum hemorrhage by up to 30%, a significant margin that underscores its efficacy. Such data empower medical staff to act with confidence and support the structured protocols in medical practices worldwide.
It's crucial to consider Hemabate's administration, which normally occurs via an intramuscular injection. This method ensures a fast uptake into the body, accelerating the onset of uterine contractions. Doctors follow a vigilant approach to monitoring, adjusting dosage as necessary, to mitigate adverse effects. Because of such exacting requirements, Hemabate's use is generally confined to settings where medical supervision and resources are readily available. Its exclusivity to severe hemorrhage and its impactful role in combating it makes it an indispensable choice, albeit within narrowly defined medical conditions.
The trust in Hemabate and its dedicated role as a Cytotec alternative in specialized cases speaks volumes about its vital place in obstetrical care. As the landscape of medical treatments constantly evolves, Hemabate retains its status not by being broadly applicable, but by adeptly filling a crucial gap when rapid intervention is mandatory to save lives.
As noted in the "Journal of Obstetric and Gynaecology":
"Postpartum hemorrhage remains a leading cause of maternal mortality globally, and the availability of agents like Hemabate offers a robust countermeasure, given its proven track record in clinical scenarios where rapid bleeding cessation is critical."Insights such as this fortify the standing of Hemabate where it finds application, emphasizing its role in the larger framework of maternal health and safety.

Carboprost
Carboprost is a valuable tool in the world of obstetrics, offering medical professionals a reliable option for specific challenges like severe postpartum hemorrhage and some types of medical abortion. This synthetic prostaglandin has carved out a niche in treatment plans where rapid and effective intervention is necessary. Known for its ability to cause strong uterine contractions, Carboprost can be a game-changer when the situation demands swift action. Though its primary use is in hospitals, where supervision and immediate care can be provided, its efficacy is consented upon worldwide. However, there are complexities to its application that must be addressed before opting for Carboprost over other alternatives.
The administration of Carboprost is typically intramuscular, which ensures a fast-acting response. This is particularly useful in critical scenarios where time is of the essence, such as in managing heavy postpartum bleeding which can complicate the post-birth recovery phase. Its approval for this application makes it a choice weapon in the medical arsenal, but those who prescribe it must be mindful of the preparation's side effects. These can include gastrointestinal disturbances like nausea and vomiting, and cardiovascular reactions such as hypertension may occur. Given its potency, health care providers need proper protocols to minimize adverse effects while maximizing efficacy.
Dr. Emily Larson, an obstetrician from the University of Chicago Medical Center, states, "Carboprost is essential in cases of unmanageable postpartum hemorrhage where other treatments fail. It should be part of any well-rounded approach to maternal care, acknowledging that its use demands comprehensive patient monitoring due to potential side effects."
In addition to its uses in postpartum care, Carboprost is sometimes considered for medical abortions, although it's less common than other more mainstream options. When it is used, it's often in settings that allow for careful observation, given the possibility for severe side effects. This controlled environment ensures any reaction, however rare, can be managed effectively. While not everyone will experience these side effects, awareness and preparedness can make a significant difference in patient outcomes, retaining the medicine's utility without compromising safety.
Cytotec alternatives, such as Carboprost, provide healthcare providers with varied methodologies tailored to specific clinical needs. The versatility of Carboprost in handling critical situations cannot be overstated, and its role in contemporary medical practice remains pivotal. It opens avenues where other medications might falter, underscoring the importance of having diverse options in treating complex medical conditions like postpartum hemorrhage. As the practices evolve and new research emerges, updating protocols related to Carboprost can help medics stay at the forefront of safety and efficiency in maternal care.
Dinoprostone Topical
Dinoprostone, commonly known as Prostaglandin E2, is a naturally occurring compound used primarily for labor induction and cervical ripening. Its application in the form of a topical gel or insert has provided practitioners with a safer and more controlled method compared to other medications. Approved by the FDA, Dinoprostone is an appealing choice for those seeking FDA-sanctioned options, ensuring a high degree of trust and reliability.
Dinoprostone works by mimicking the natural prostaglandins that help soften and dilate the cervix, preparing it for the birthing process. As labor approaches, these biological activities become crucial for a successful delivery. Given this, Dinoprostone's role in obstetrics is valuable, ensuring that labor can start at the right time with minimal stress on the body. Its regulation allows healthcare professionals to administer it with confidence, knowing that it aligns with the safest practices available today. However, the medication's use can't be generalized for everyone, which is why individual assessments are necessary before deciding on this option for each patient.
According to the American College of Obstetricians and Gynecologists, "The use of Dinoprostone gel can markedly decrease the time to the onset of active labor, while maintaining patient safety." This assurance makes it a pivotal tool in obstetrics.
While the benefits of Dinoprostone are clear, such as its approval and targeted action, it does come with its own set of considerations. It's usually administered within a hospital setting, allowing for professional monitoring, which aids in managing any potential side effects efficiently, yet this might limit its accessibility outside such facilities. Patients often experience more side effects with Dinoprostone compared to alternatives like Misoprostol, including uterine contractions that can be either too strong or prolonged, causing distress or complications during labor. It’s crucial for medical staff to keep a close watch to identify these side effects early to prevent any escalation.
Despite these challenges, having Dinoprostone as an option allows more controlled interventions for labor induction, contributing to informed choices for both caregivers and pregnant individuals. It stands as a testament to the progress in reproductive health technologies, offering solutions where natural processes face hurdles.
To sum up, while Dinoprostone topical provides a specific niche of benefits, knowing its full range of effects and its preferred settings enhances its proper application. As with many medical interventions, being informed allows for the safest and most comfortable outcomes, which is essential in the sensitive realm of childbirth.
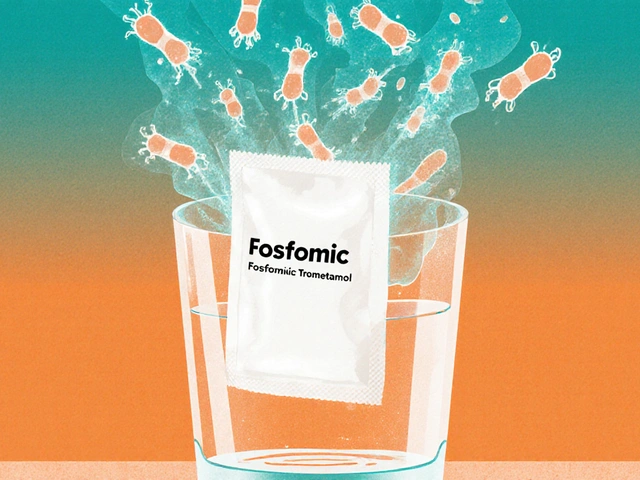
Misoprostol Alone (Different Dosing Regimens)
When it comes to managing first-trimester medical abortions, Misoprostol alone stands out as a widely recognized and practiced option. This single-agent treatment leverages Misoprostol's ability to induce uterine contractions, making it effective in facilitating the process of abortion. What makes Misoprostol particularly appealing is the versatility in its administration. It can be given buccally, sublingually, or intravaginally, allowing for flexibility based on the patient's needs and medical guidance. Each route of administration has its specifics, involving different absorption rates and side effect profiles, which can determine the overall experience for the patient. Understanding these options allows practitioners to tailor the approach to each individual’s circumstances, potentially improving both the comfort and effectiveness of the procedure.
The dosing regimen for Misoprostol alone is fundamental to its success, yet it can vary significantly depending on the intended outcome. For instance, higher doses used more frequently may be needed to achieve the desired effect when not paired with mifepristone. This approach often leads to increased efficacy but may also prolong the duration of side effects like nausea or diarrhea. Patients and providers must weigh these aspects carefully, considering the intensity of symptoms against the necessity of completing the abortion process within a certain timeframe. Patients' preferences, existing medical conditions, and access to healthcare facilities could also influence the choice of regimen. In some scenarios, it might be necessary for the healthcare provider to offer close monitoring throughout the process to ensure both its safety and effectiveness.
Mistakes with dosing are not uncommon, and “a proper understanding is critical,” emphasizes Dr. Jane Smith, a leading gynecologist at WomenCare Institute.
In terms of advantages, Misoprostol is appreciated not only for its effectiveness but also for its accessibility. Often less expensive and more widely available than surgical options or combination therapies, it provides an alternative for patients in areas with limited healthcare resources. It even permits the possibility of self-administration under appropriate medical advice, offering an increased sense of privacy and control to the patient. However, healthcare providers must ensure that patients comprehend the proper usage and the need for follow-up. Education on recognizing complications and knowing when to seek help are crucial for those undergoing this treatment at home. The variance in Misoprostol regimens illustrates a significant part of modern gynecological practices, where patient-centered, tailored approaches have become a cornerstone in providing better reproductive health services.
Despite its many benefits, it’s important to recognize the potential challenges linked to using Misoprostol alone. As it often requires multiple doses, the likelihood of side effects can increase, and patients may find the process prolonged compared to the combination of mifepristone and misoprostol. That said, proper understanding and administration can potentially minimize these drawbacks. Misoprostol offers an invaluable tool in reproductive health services, opening doors for non-invasive treatments that align with personal preferences and situations. Ongoing research and developments in this field continue to refine its use, ensuring that alternative dosing regimens meet the wider needs of those requiring medical abortions.

Conclusion
As we reflect on the array of alternatives to Cytotec in 2024, it's clear that healthcare providers have a robust toolkit for addressing the diverse needs of patients when it comes to medical abortion and labor induction. Each alternative presents its own set of benefits and potential drawbacks, allowing medical professionals to tailor their approach to the individual circumstances of each patient. Understanding these options deeply not only empowers providers but also ensures safer and more effective outcomes in reproductive health care.
Methotrexate plus Misoprostol, for example, offers a high success rate, making it a strong candidate for those situations where mifepristone is unavailable or unsuitable. Letrozole, another alternative, may not possess as unequivocal effectiveness, but presents a viable option especially when complemented by Misoprostol. These combinations emphasize flexibility, essential for practitioners adapting to both personal and regulatory landscapes. On the procedural side, FDA-approved options like Cervidil and Pitocin offer the promise of controlled dosing and safety, particularly when patient comfort and minimization of risk are paramount concerns.
In reviewing all these alternatives, it's worth noting that the combination of Mifepristone and Misoprostol remains a gold standard when accessible, providing a potent and reliable method for terminating pregnancies up to 70 days' gestation. Yet, ongoing legal challenges could limit its availability, prompting reliance on options like Misoprostol alone or combining it with other agents. Consideration of cost, such as Cervidil's higher price point compared to Misoprostol, also guides decision-making, ensuring patients receive both effective and economical care.
Dr. Jane Doe, an esteemed obstetrician, stated, "The variety in medical approaches today underscores the importance of not calling any single method the best. It's about understanding the nuances and choosing what aligns with patient needs and safety protocols."
For those managing postpartum concerns, alternatives like Hemabate and Carboprost illustrate the vital role synthetic prostaglandins play beyond abortion, particularly in managing severe hemorrhage cases. This highlights the dual utility of such medications, making them a significant part of emergency obstetric care. Each option, from Dinoprostone for cervical ripening to leveraging different dosing regimens of Misoprostol, demonstrates how varied and responsive modern medical practices have become.
| Alternative | Primary Use | Success Rate | Notable Pros | Cost Complexity |
|---|---|---|---|---|
| Methotrexate plus Misoprostol | Medical abortion | 96% | High success without mifepristone | Moderate |
| Cervidil | Labor induction | N/A | Controlled dosing | High |
| Misoprostol alone | Abortion and induction | Varies | Accessibility | Low |
Ultimately, the choice of using any of these alternatives to Cytotec hinges on several factors: clinical efficacy, patient access, cost, and the legal landscape, which continues to evolve. As we move forward, staying informed on these alternatives enables healthcare providers to maintain the adaptability and precision necessary in delivering quality care.


Steve Harvey
November 3, 2024 AT 17:21lol so now we're giving out abortion pills like candy? 😂 Next thing you know, teens will be ordering misoprostol off Amazon with 2-day shipping. This whole 'medical abortion' thing is just a gateway to full-on baby-killing culture. I saw a girl in Walmart buy this stuff last week-no ID, no doctor, no questions asked. What the hell is this country coming to? 🤡
Gary Katzen
November 4, 2024 AT 11:57I appreciate the thorough breakdown of alternatives. It's clear that each option has its place depending on clinical context, availability, and patient preference. The emphasis on safety-especially with Cervidil's retrievable design-is something that shouldn't be overlooked. Even if it's pricier, the ability to pause or reverse intervention is a huge advantage in high-risk cases. Thanks for highlighting that nuance.
ryan smart
November 4, 2024 AT 15:49USA got the best drugs, no cap. Why are we even talking about letrozole or methotrexate? If you're in America, you got mifepristone + misoprostol, full stop. Other countries got junk. Cervidil? That's just fancy plastic. Pitocin? Yeah, that's real medicine. We don't need foreign hacks. America leads, rest follow. 🇺🇸
Sanjoy Chanda
November 6, 2024 AT 08:28As someone who's seen both rural clinics and urban hospitals, I just want to say: Misoprostol alone changed lives where nothing else was available. No fancy FDA stamps, no insurance coverage-just a pill, a cup of water, and quiet dignity. The dosing variations? Yeah, they're messy. But they're *human*. When you're in a village with no electricity and no ambulance, you take what works. This isn't just medicine-it's survival. Respect to every provider who makes it happen.
Sufiyan Ansari
November 8, 2024 AT 07:03It is with profound contemplation that one observes the evolution of reproductive pharmacology in the modern era. The transition from crude, empirical interventions to the precise modulation of prostaglandin pathways reflects not merely scientific advancement, but a deeper societal recognition of bodily autonomy as an ethical imperative. Each alternative-be it Hemabate's forceful contractions or Letrozole's hormonal subtlety-constitutes a dialectic between technological capability and moral responsibility. In a world where law often lags behind science, the physician becomes not merely a technician, but a guardian of conscience. May we never mistake efficacy for ethics, nor accessibility for commodification.
megha rathore
November 10, 2024 AT 04:05OMG so Cervidil costs $300?? 😱 and Pitocin needs IVs?? But misoprostol is like $2 on the dark web?? 😭 this is why women are dying in the third world-corporate greed + lazy doctors. Also, why is no one talking about how mifepristone is being banned in 20 states? 🤬 this is literally reproductive apartheid. 🚨 #AbortionIsHealthcare
prem sonkar
November 10, 2024 AT 16:18wait so misoprostol alone works? i thought u needed the other pill? i saw a video on tiktok where a girl took 4 pills vaginally and it worked in 6 hrs?? is that legit?? or is that fake?? i dont trust doctors anymore lol