Link Between Meniere's Disease and Vision Issues
If you’ve been diagnosed with Meniere’s, you probably know the classic trio: ringing ears, dizzy spells, and hearing loss. What many don’t expect is that your eyes can join the party. A lot of patients report blurry vision, eye‑movement glitches, or the feeling that the room is shifting right before a vertigo attack. That’s not random – the inner ear and the eyes talk to each other all the time.
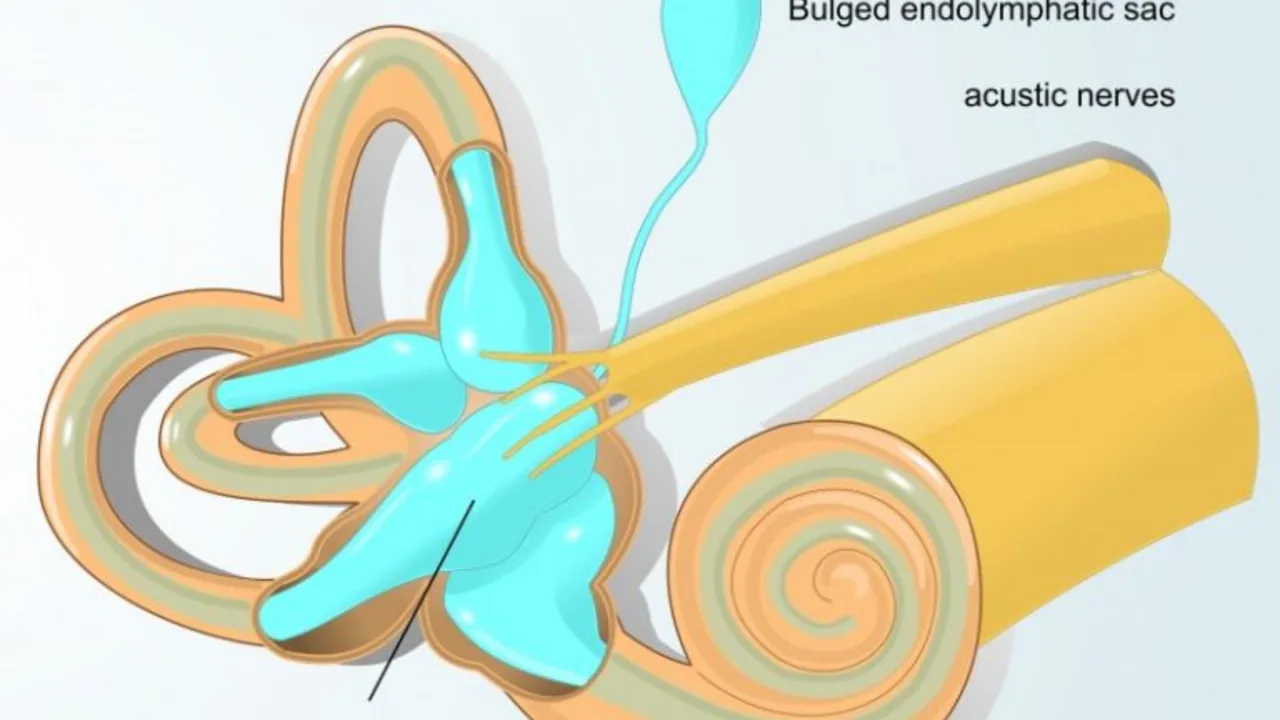
The inner ear houses the vestibular system, which tells your brain where your head is in space. Your eyes use that info to keep the world steady on the retina. When the vestibular system goes haywire during a Meniere’s flare‑up, the visual system gets confused. The result can be what doctors call "visual vertigo" – the sensation that the environment is moving even though you’re standing still.
Why Vision Can Be Affected
First, the vestibulo‑ocular reflex (VOR) is a fast‑acting loop that stabilizes your gaze when you move. If the fluid pressure in the cochlea spikes, the VOR can send mixed signals, leading to nystagmus (rapid eye twitching) or temporary double vision. Second, some Meniere’s medications, especially diuretics or steroids, can change blood sugar or blood pressure, which in turn can blur vision. Third, the stress and anxiety that come with frequent attacks can cause eye strain – think of it like a muscle cramp but for the muscles that move your eyes.
Research shows that about 30‑40 % of people with Meniere’s notice some visual disturbance during an episode. It’s not a permanent loss of sight, but it can be scary in the moment. The key is to recognize the pattern: vision changes that line up with ringing ears or spinning sensations are usually tied to your vestibular system, not an eye disease.
What You Can Do About It
Start by tracking your symptoms. Keep a simple diary – note the time of a vertigo spell, what you saw (blur, double, tunnel vision), and any meds you took. That paper trail helps your doctor decide whether a medication tweak or a vestibular rehab program is needed.
If you’re on diuretics like hydrochlorothiazide, ask your doctor if a lower dose might reduce eye‑related side effects. Some clinicians also prescribe low‑dose betahistine to improve inner‑ear blood flow, which can calm both ear and eye symptoms.
Vestibular rehabilitation therapy (VRT) is a set of exercises that trains the brain to rely less on the faulty inner‑ear input and more on visual cues. Simple VRT moves – like focusing on a dot while turning your head – can lessen the visual fog after an attack. A physical therapist can tailor a program to your needs.
Don’t ignore eye‑specific care. If you wear glasses, make sure your prescription is up‑to‑date; a slight change in refraction can make visual vertigo feel worse. When you feel a flare‑up coming, sit down, close your eyes for a few seconds, and let the VOR settle before you try to walk or drive.
Lastly, stay hydrated and watch your salt intake. Reducing fluid buildup in the inner ear can lower the frequency of attacks, which in turn cuts down on vision disturbances.
Bottom line: Meniere’s isn’t just an ear problem. Your eyes are part of the same balance network, so it’s normal to see visual quirks when the inner ear misfires. By logging symptoms, tweaking meds, and doing targeted exercises, you can keep both your hearing and sight steadier.
Meniere's Disease and Vision: Understanding the Link
Hey there, beautiful souls! Today we're going to explore a unique topic, the connection between Meniere's Disease and vision problems. Often overlooked, this correlation is quite significant, increasing our understanding of how Meniere's Disease affects our day-to-day lives. We'll dive into the symptoms, causes, and ways to manage these visual disruptions caused by this condition. Stick with me, and let's reveal these insights together.

Gallstones and Mental Health: Coping with the Stress
Feb, 19 2025