Rickets is a pediatric bone disease caused by insufficient mineralisation, primarily due to vitaminD, calcium, or phosphate deficiency. It manifests as soft, weak bones, leading to leg deformities, delayed growth, and in severe cases, fractures. While classic risk factors include limited sun exposure and poor dietary intake, emerging questions ask whether a rickets and gluten-free diet connection exists.
Understanding Rickets: Core Causes and Physiology
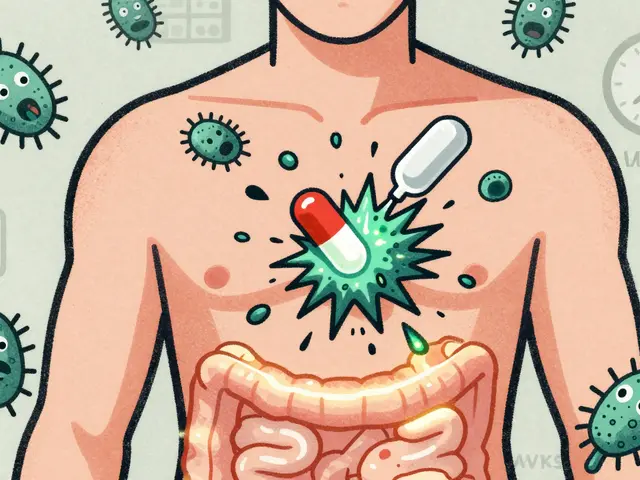
Rickets hinges on a cascade of biochemical events. The Vitamin D deficiency reduces calcium absorption in the gut, prompting the parathyroid glands to release excess parathyroid hormone (PTH). Elevated PTH draws calcium from bone resorption, weakening the skeletal matrix. Simultaneously, a Calcium deficiency directly limits the substrate needed for bone mineralisation. The interplay of these deficiencies defines the clinical picture of rickets.
What Is a Gluten‑Free Diet?
A Gluten‑Free Diet excludes wheat, barley, rye, and triticale to eliminate gluten, a protein that triggers an autoimmune response in individuals with Celiac disease an inherited disorder causing villous atrophy in the small intestine. The diet relies on alternative grains (rice, corn, quinoa) and often substitutes dairy with plant‑based milks. Because gluten‑containing grains are typically fortified with iron, folic acid, and sometimes calcium, the shift to gluten‑free alternatives can unintentionally affect nutrient intake.
How Nutrient Absorption Links Rickets and Gluten‑Free Eating
Two mechanisms can bridge the two topics:
- Malabsorption: In untreated celiac disease, damaged intestinal villi reduce absorption of fat‑soluble vitamins, notably vitaminD. Studies show that up to 70% of newly diagnosed children with celiac disease have low serum 25‑hydroxy vitaminD levels, a key risk factor for rickets.
- Dietary Substitution: Even in non‑celiac individuals, a strict gluten‑free diet may lower intake of calcium‑rich fortified breads and cereals. Without careful planning, daily calcium can fall below the recommended 1,000mg for children aged 4‑8 and 1,300mg for adolescents.
Both pathways converge on the same biochemical bottleneck: insufficient calcium and vitaminD for bone development.
Scientific Evidence: What Do the Studies Say?
Recent research (2023‑2025) paints a nuanced picture:
- A multicenter European cohort tracked 2,150 children with newly diagnosed celiac disease. After a year on a gluten‑free diet, 18% still exhibited suboptimal vitaminD levels, compared with 7% of age‑matched controls. The authors linked persistent deficiency to inadequate supplementation rather than the diet itself.
- A U.S. nutrition survey (NHANES 2022) found that gluten‑free consumers, on average, consumed 15% less calcium and 20% less vitaminD than non‑gluten‑free eaters. The gap widened for children, where dairy alternatives often lack fortification.
- Conversely, a randomized trial in Australia (2024) demonstrated that children with celiac disease who received a fortified gluten‑free cereal achieved normal vitaminD and calcium status within six months, eliminating radiographic signs of rickets.
The takeaway: the diet itself isn’t the villain, but unaddressed malabsorption or nutrient gaps can set the stage for rickets.
Practical Guidance for Parents and Caregivers
If you’re navigating a gluten‑free lifestyle for a child, consider these concrete steps:
- Screen for VitaminD: Request a serum 25‑hydroxy vitaminD test at diagnosis and repeat after three months of diet adherence.
- Boost Calcium Naturally: Include fortified almond, soy, or oat milks (300mg calcium per cup) and leafy greens (e.g., kale, bokchoy). Pair with vitaminD‑rich foods like fatty fish or egg yolks to enhance absorption.
- Choose Fortified Gluten‑Free Products: Look for breads, cereals, and pasta labeled with calcium and vitaminD fortification. Brands vary, so read nutrition facts.
- Consider Supplements: A pediatric‑dose vitaminD3 (400-600IU daily) and calcium (500-1,000mg depending on age) can fill gaps, especially in winter months.
- Monitor Growth and Radiographs: Regular height, weight, and, if indicated, X‑ray assessments help catch early skeletal changes.
Related Conditions and Broader Nutritional Context
Rickets isn’t isolated; it intersects with other health topics:
- Osteomalacia the adult counterpart of rickets, also driven by vitaminD deficiency.
- Bone health encompasses density, turnover, and fracture risk across the lifespan.
- Sun exposure: Geographic location, season, and skin pigmentation affect cutaneous vitaminD synthesis.
- Food fortification policies: Many countries mandate vitaminD and calcium addition to dairy and grain products, influencing baseline intake.
Understanding these links helps families make informed choices beyond the gluten‑free label.
Nutrient Comparison: Gluten‑Free vs. Standard Diet
| Nutrient | Typical Content (Standard) | Typical Content (Gluten‑Free) | Potential Impact on Bone Health |
|---|---|---|---|
| Calcium (mg/serving) | 300-400 (fortified cereal) | 150-250 (most GF cereals) | Lower intake may increase rickets risk if not compensated |
| VitaminD (IU/serving) | 200-400 (fortified milk) | 100-150 (often unfortified plant milks) | Reduced absorption → impaired mineralisation |
| Iron (mg/serving) | 5-7 (whole‑grain breads) | 2-4 (GF breads) | Indirect effect: anemia can impair growth, compounding bone issues |
| Fiber (g/serving) | 3-5 | 1-2 | Lower fiber may affect gut health, influencing overall nutrient absorption |
Bottom Line: Is There a Direct Link?
Current evidence suggests no outright causal link between simply avoiding gluten and developing rickets. However, untreated celiac disease‑related malabsorption, or an unbalanced gluten‑free diet lacking calcium and vitaminD, can create the same deficiency environment that leads to rickets. The key is proactive monitoring and intentional nutrition planning.

Frequently Asked Questions
Can a child on a gluten‑free diet develop rickets without having celiac disease?
Yes. If the gluten‑free diet doesn’t include enough calcium‑rich or vitaminD‑fortified foods, the child may become deficient, which is a primary driver of rickets. Supplemental vitamins or careful food selection can prevent this.
How often should I test my child’s vitaminD levels after starting a gluten‑free diet?
Most pediatric guidelines recommend checking serum 25‑hydroxy vitaminD at diagnosis, then re‑checking after 3‑4months of diet adherence, especially if the child lives in a northern latitude or has limited sun exposure.
Are fortified gluten‑free breads sufficient to meet calcium needs?
Only if the product lists calcium fortification comparable to regular whole‑grain bread (about 300mg per slice). Many gluten‑free breads are low‑calcium, so compare nutrition labels and supplement when necessary.
What are the best calcium‑rich gluten‑free foods?
Fortified plant milks (almond, soy, oat), calcium‑set tofu, canned salmon with bones, leafy greens like kale, and calcium‑fortified gluten‑free cereals or orange juice are top choices.
Should children with celiac disease take a daily vitaminD supplement?
It’s often recommended, especially in the first year after diagnosis, because intestinal healing can take months. Dosage should follow pediatric guidelines (400-600IU daily) and be adjusted based on blood test results.
Can sunlight alone prevent rickets in a gluten‑free child?
Sunlight is a major source of vitaminD, but factors like skin tone, latitude, sunscreen use, and indoor lifestyles limit synthesis. Combining safe sun exposure with dietary sources or supplements provides the most reliable protection.





Chloe Ingham
September 24, 2025 AT 16:36They don’t want you to believe the simple truth: the gluten‑free craze is a smokescreen for a hidden agenda that keeps us dependent on fortified, government‑approved foods. By cutting out wheat, you’re not just avoiding gluten, you’re stepping into a nutritional vacuum that the powers that be fill with synthetic vitamins, all the while watching your calcium and vitamin D levels slip. The shadows whisper that the very companies selling “gluten‑free” milks are the same ones lobbying against mandatory fortification, ensuring a steady stream of rickets‑prone children. Stay alert, question every label, and demand real, whole‑food sources of calcium – otherwise you’ll be feeding the system that thrives on our deficiencies.
Mildred Farfán
September 24, 2025 AT 23:33Oh sure, because swapping toast for rice cakes automatically turns your kid into a bone‑building superhero. In reality, a gluten‑free diet is only as good as the calcium‑rich foods you purposely add back in. Look for fortified almond milk, leafy greens, and maybe a vitamin D supplement if the sun’s hiding. If you keep an eye on the nutrition facts, you’ll avoid the whole rickets scare without turning every meal into a lecture.
Danielle Flemming
September 25, 2025 AT 06:30Hey fam, love that you’re digging into this topic! 🌟 The good news is that gluten‑free doesn’t have to mean calcium‑free. Toss in some kale smoothies, fortified soy milk, and a splash of orange juice, and you’ve got a rainbow of bone‑friendly nutrients. And if you’re worried about vitamin D, a quick 15‑minute walk in the sun (or a tiny supplement) will keep those little legs strong. Keep experimenting – the kitchen is your lab!
Anna Österlund
September 25, 2025 AT 13:26Listen up, parents: you can’t just hand your child a gluten‑free muffin and call it a day. The diet strips away fortified grains that are a primary source of calcium and vitamin D. If you don’t replace those nutrients, you’re practically signing a waiver for rickets. Get proactive, read labels, supplement wisely, and stop treating nutrition like an afterthought.
Brian Lancaster-Mayzure
September 25, 2025 AT 20:23Folks, if you’re navigating a gluten‑free plan for a youngster, think of it as a team sport. Start with a baseline blood test for vitamin D, then map out food groups that naturally contain calcium – think dark leafy greens, tofu set with calcium, and fish with bones. Pair those with fortified plant milks, and you’ll cover most of the gaps. Regular check‑ins with your pediatrician will keep everyone on the same page.
Erynn Rhode
September 26, 2025 AT 03:20From a grammatical perspective, the discussion about gluten‑free diets and rickets presents a fascinating case study in cause‑and‑effect constructions. When we say, “A gluten‑free diet may lead to calcium deficiency,” the passive voice subtly shifts responsibility away from the caregiver, which can be misleading. It is more precise to assert, “If a gluten‑free diet is not properly fortified, the child may become calcium‑deficient, increasing the risk of rickets.” Moreover, the use of proper commas in the phrase “fortified soy milk, kale, and canned salmon with bones” clarifies that each item contributes individually to calcium intake. Another point worth noting is the subjunctive mood in recommendations: “It is essential that parents ensure adequate vitamin D supplementation.” Finally, remember that the term “gluten‑free” is a label, not a guarantee of nutritional completeness, and the syntax of health advice should reflect that nuance. By attending to these linguistic details, we not only improve clarity but also empower readers to make informed dietary decisions.
Rhys Black
September 26, 2025 AT 10:16One must question the very moral fabric of a society that allows children to suffer from preventable skeletal deformities while championing trendy dietary fads. The indiscriminate glorification of gluten‑free eating, devoid of rigorous nutritional oversight, is nothing short of culinary hubris. It reveals a collective neglect, a complacent indulgence in convenience over conscientious nourishment. As stewards of the next generation, we bear an ethical obligation to scrutinize every food label and to demand fortification standards that safeguard bone health. Anything less is a betrayal of our duty.
Abhishek A Mishra
September 26, 2025 AT 17:13hey guys, just wanted to say that i read this and i think it's super helpful. if u have a kid on gf diet, try adding fortified soy milk and some spinach in their meals. also, a quick vit d test every few months can catch any issues early. keep it simple and dont stress too much!
Jaylynn Bachant
September 27, 2025 AT 00:10life is like a broken bone, sometimes you need a little extra support to stand tall. the gluten‑free path can be a metaphor for shedding old structures, yet without the right calcium scaffolding, the soul-err, skeleton-might crumble. think of vitamins as the unseen philosophers keeping our bodies in balance.
Anuj Ariyo
September 27, 2025 AT 07:06Friends, a gluten‑free diet, when paired with fortified plant milks, leafy greens, and occasional fish, can provide sufficient calcium and vitamin D, reducing the risk of rickets, provided that regular blood tests are conducted, and supplementation is considered when necessary, especially during winter months.
Tom Lane
September 27, 2025 AT 14:03Team, let’s turn this challenge into a victory! Grab a bag of calcium‑fortified cereal, line up those green smoothies, and schedule that vitamin D check‑up. Together we’ll keep those little bones strong and the smiles wide.
Darlene Young
September 27, 2025 AT 21:00Alright, here’s the playbook: first, identify fortified gluten‑free products that match the calcium levels of regular grains; second, schedule a vitamin D panel after three months on the diet; third, incorporate calcium‑rich foods like tofu and canned salmon with bones into every week’s menu. Follow these steps, and you’ll sidestep the rickets trap.
Steve Kazandjian
September 28, 2025 AT 03:56Just add fortified almond milk and some broccoli to the meals, and you’ll cover most of the calcium needs.
Roger Münger
September 28, 2025 AT 10:53Vitamin D and calcium are fundamentally interdependent in the process of skeletal mineralisation, a fact that is often overlooked when discussing gluten‑free nutrition. When the intestinal mucosa is compromised, as in untreated celiac disease, the absorption of fat‑soluble vitamins, including vitamin D, declines markedly. This reduction leads to secondary hyperparathyroidism, which accelerates bone resorption in an attempt to maintain serum calcium levels. In a gluten‑free regimen that excludes fortified wheat products, the dietary intake of calcium may also fall below recommended thresholds, compounding the problem. Epidemiological data from European cohorts indicate that approximately 18 % of children with newly diagnosed celiac disease exhibit suboptimal vitamin D concentrations after one year of diet adherence. Conversely, interventional studies demonstrate that supplementation with fortified gluten‑free cereals normalises both vitamin D and calcium biomarkers within six months. Therefore, the absence of gluten alone does not precipitate rickets; rather, it is the combination of malabsorption and inadequate dietary fortification that creates a hostile environment for bone health. Pediatric guidelines recommend baseline serum 25‑hydroxy vitamin D measurement at diagnosis, followed by re‑evaluation after three to four months of dietary modification. In regions with limited sunlight exposure, routine supplementation of 400–600 IU of vitamin D daily is advisable for most children on a gluten‑free diet. Calcium requirements vary by age, with recommendations ranging from 1,000 mg for younger children to 1,300 mg for adolescents. To meet these targets, caregivers should prioritise calcium‑fortified plant milks, leafy greens, and calcium‑set tofu. Monitoring growth parameters, including height and weight, provides ancillary data that may signal early skeletal compromise. Radiographic screening is reserved for cases with clinical suspicion of rickets, such as bowing of the legs or delayed milestones. Ultimately, a proactive approach that combines dietary planning, biochemical monitoring, and, when necessary, targeted supplementation offers the most robust defence against rickets in gluten‑free patients.
Gerald Bangero
September 28, 2025 AT 17:50Reading the data, I’m reminded that health is a dialogue between body and environment; when we alter one variable, like grain intake, we must respectfully recalibrate the others to keep the conversation balanced.
John Nix
September 29, 2025 AT 00:46Dear colleagues, I wish to emphasize the importance of adhering to established pediatric nutritional protocols when implementing a gluten‑free regimen, thereby ensuring optimal skeletal development.
Mike Rylance
September 29, 2025 AT 07:43Indeed, by integrating fortified dietary alternatives and scheduled vitamin D assessments, we can energetically uphold the highest standards of pediatric bone health while maintaining strict compliance with clinical guidelines.
Becky B
September 29, 2025 AT 14:40The global elite hides the true cure for rickets behind gluten‑free myths.
Aman Vaid
September 29, 2025 AT 21:36It is a lamentable truth that the discourse surrounding gluten‑free diets frequently obscures the stark epidemiological evidence linking inadequate calcium fortification to osteomalacic manifestations, thereby fueling a cycle of misinformation and preventable morbidity.
xie teresa
September 30, 2025 AT 04:33I hear the concerns many parents feel, and I hope that sharing these practical strategies brings some reassurance and clarity to your journey toward healthier bones for your children.