Obesity and RCC Risk Calculator
Enter Your Information
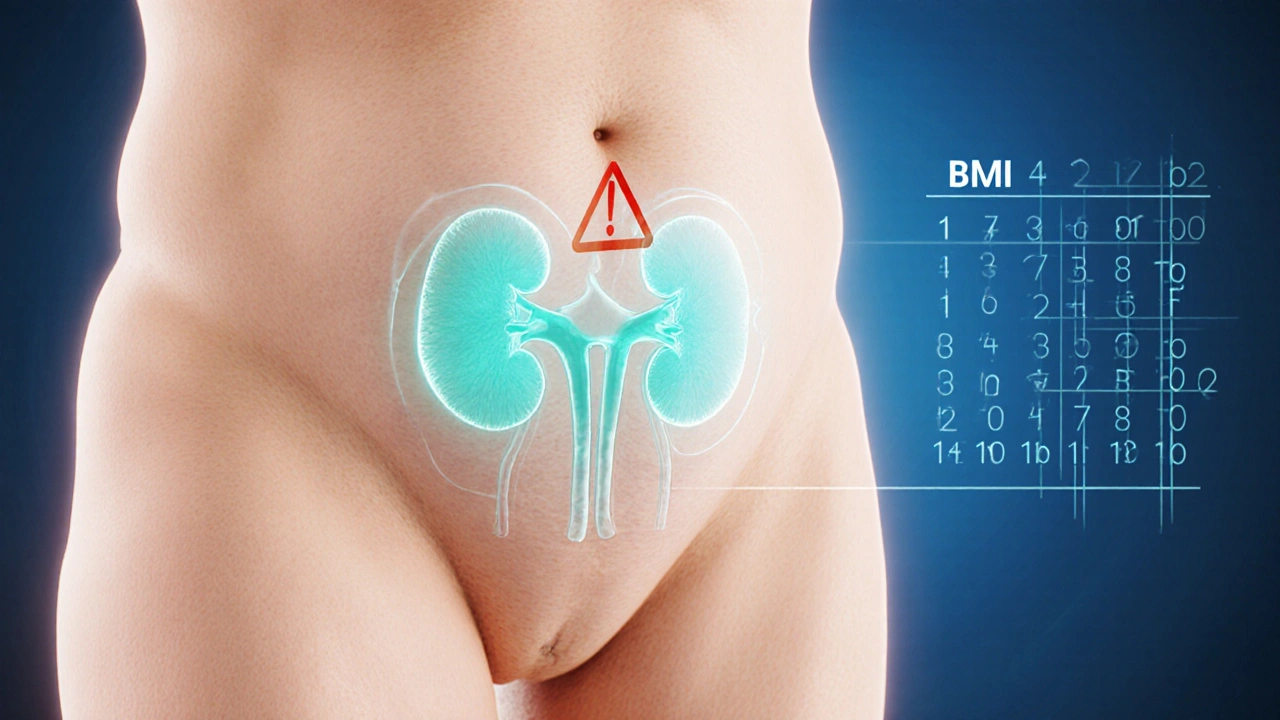
This calculator estimates your risk of developing advanced renal cell carcinoma based on body mass index and other factors.
Your Risk Assessment
When you hear the word "cancer," the first thing that comes to mind is often a tumor in the lung, breast, or colon. But kidney cancer - specifically renal cell carcinoma (RCC) - accounts for about 90% of all kidney malignancies, and its incidence has been climbing worldwide. A growing body of research shows that excess body weight isn’t just a cosmetic concern; it can dramatically raise the odds of developing an obesity and renal cell carcinoma risk that progresses to an advanced stage.
Key Takeaways
- Obesity roughly doubles the risk of being diagnosed with RCC compared with normal‑weight individuals.
- The link is strongest for advanced (stageIII‑IV) disease, where obese patients face a 30‑50% higher chance of poor outcomes.
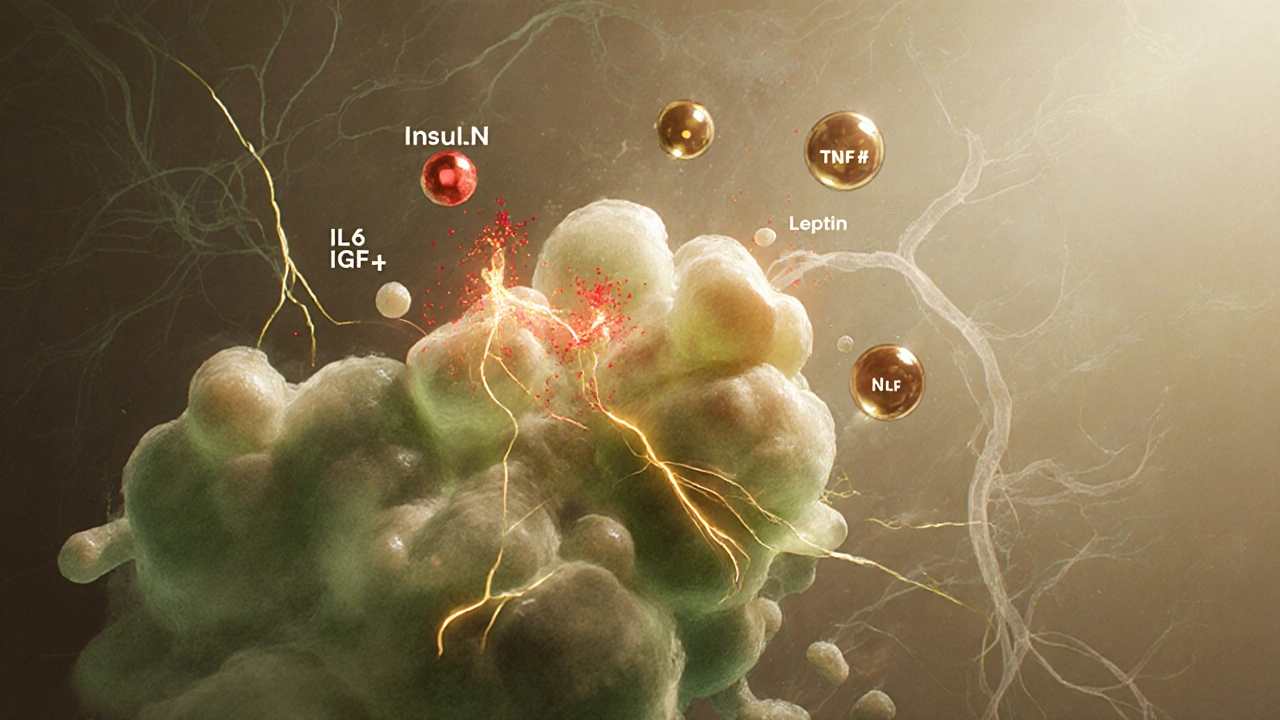
- Biological mechanisms include altered insulin signaling, chronic inflammation, and changes in the tumor microenvironment.
- Population studies from the U.S., Europe, and Asia consistently report odds ratios between 1.5 and 2.3 for RCC in obese cohorts.
- Weight‑management, regular screening for high‑risk groups, and early‑stage treatment can dramatically improve survival.
Understanding Obesity
Obesity is a chronic condition characterized by excess body fat, typically defined by a body mass index (BMI) of 30kg/m² or higher. While BMI is a simple calculation-weight (kg) divided by height (m) squared-it remains the most widely used metric in epidemiological studies because it correlates well with adiposity and health risk.
Beyond the sheer amount of fat, obesity triggers a cascade of hormonal and metabolic changes: higher circulating insulin, increased leptin, and a persistent low‑grade inflammatory state. These shifts set the stage for cellular environments that favor tumor growth.
What Is Renal Cell Carcinoma?
Renal Cell Carcinoma is the most common type of kidney cancer, arising from the lining of the proximal tubules in the kidney. RCC is staged from I (localized) to IV (metastatic). When the disease reaches stageIII or IV, it is often referred to as Advanced Renal Cell Carcinoma (advanced RCC), indicating that the tumor has either invaded major blood vessels, spread to nearby organs, or metastasized to distant sites such as the lungs, bone, or brain.
Advanced RCC carries a markedly lower 5‑year survival rate-about 12-15%-compared with the >90% survival for early‑stage disease.
How Obesity Fuels RCC Development
Researchers have pinpointed several pathways that explain why excess weight boosts RCC risk:
- Insulin and IGF‑1 surge: High insulin levels stimulate the insulin‑like growth factor‑1 (IGF‑1) pathway, which promotes cell proliferation and inhibits apoptosis (programmed cell death). RCC cells are particularly sensitive to IGF‑1 signaling.
- Chronic inflammation: Adipose tissue secretes cytokines such as IL‑6, TNF‑α, and CRP. Persistent inflammation creates DNA damage and encourages angiogenesis-the formation of new blood vessels that feed tumors.
- Altered adipokine profile: Leptin (often elevated in obesity) has pro‑angiogenic effects, while adiponectin (usually reduced) normally protects against tumor growth.
- Renal lipid accumulation: Fat deposits around the kidneys can cause lipotoxicity, leading to oxidative stress and genetic mutations within renal tubular cells.
- Hormonal imbalances: Obesity can increase estrogen and aromatase activity, both of which have been linked to higher RCC incidence.
These mechanisms don’t act in isolation; they intertwine to create a microenvironment that’s ripe for cancer initiation and progression.
Epidemiological Evidence: Numbers That Speak
Large‑scale cohort studies consistently show a dose‑response relationship between BMI and RCC risk. Below is a snapshot of findings from three major analyses published between 2018 and 2023.
| Study | BMI Category | OR (95% CI) | Population |
|---|---|---|---|
| US Nurses' Health Study (2020) | 30-34.9kg/m² | 1.62 (1.34-1.95) | Female nurses, 1990‑2018 |
| European Prospective Investigation (2019) | ≥35kg/m² | 2.03 (1.71-2.40) | Men & women, 8countries |
| Asian Cohort Study (2021) | 25-29.9kg/m² (overweight) | 1.38 (1.10-1.73) | Urban adults, China & Japan |
When researchers drill down to advanced disease, the odds ratios tend to rise. A meta‑analysis of 12 studies involving over 1million participants reported an OR of 2.45 (95%CI1.89‑3.18) for stageIII-IV RCC among individuals with BMI≥30kg/m².
What Advanced RCC Means for Patients
Advanced RCC is not just a bigger tumor; it represents a shift in biology:
- Higher tumor grade: Cells are more aggressive and less differentiated.
- Increased metastasis: Cancer spreads through the renal vein to the lungs, bones, and brain.
- Reduced Survival Rate: Five‑year overall survival drops below 20% without systemic therapy.
Treatment typically involves a combination of nephrectomy (removal of the kidney), targeted therapies (e.g., VEGF inhibitors), and newer immunotherapies such as PD‑1 checkpoint blockers. However, obese patients may experience higher rates of treatment‑related toxicity, making personalized dosing crucial.

Reducing Your Risk: Practical Steps
Whether you’re already carrying extra pounds or aiming to maintain a healthy weight, the following actions can lower your odds of developing RCC, especially in its advanced form:
- Adopt a Mediterranean‑style diet: Emphasize vegetables, whole grains, legumes, nuts, and olive oil. Studies link this pattern to a 20% reduction in renal cancer incidence.
- Engage in regular aerobic activity: Aim for at least 150minutes of moderate‑intensity exercise per week. Even modest weight loss (5‑10%) can normalize insulin levels.
- Monitor your Body Mass Index annually. Use a reliable scale and stadiometer; keep a chart of trends.
- Get screened if you’re high‑risk: Adults over 50 with a BMI≥30, a family history of kidney cancer, or chronic hypertension should discuss abdominal imaging (ultrasound or low‑dose CT) with their physician.
- Control blood pressure and diabetes: Both conditions independently raise RCC risk; effective management reduces inflammatory load.
- Avoid tobacco and limit alcohol: Smoking doubles RCC risk, and heavy alcohol use adds to renal stress.
Checklist: What to Track If You’re Concerned About RCC
- Current weight and BMI - update every 6months.
- Blood pressure readings - aim for <130/80mmHg.
- Fasting glucose or HbA1c - keep within normal range.
- Family history of kidney or other cancers - note dates and relation.
- Any new flank pain, blood in urine, or unexplained weight loss - report promptly.
- Results of any abdominal imaging - keep copies for future reference.
Keeping this information handy makes conversations with your healthcare provider more productive and can help spot red flags early.
Frequently Asked Questions
Does losing weight lower my RCC risk?
Yes. Research shows that even a 5‑10% reduction in body weight improves insulin sensitivity and reduces inflammatory markers, which together can cut RCC risk by roughly 15‑20%.
Is BMI the only metric doctors use to assess risk?
BMI is a convenient screen, but doctors also look at waist‑to‑hip ratio, visceral fat measured by imaging, and metabolic labs (glucose, lipids) to gauge cancer‑related risk.
Can a healthy diet protect me if I’m already obese?
Diet alone won’t erase the existing risk, but shifting to a plant‑rich, low‑processed‑food regimen can slow disease progression and improve treatment tolerance.
Should I get regular kidney scans even without symptoms?
Screening isn’t universally recommended, but high‑risk groups-obese adults over 50 with hypertension or a family history-should discuss periodic ultrasound or low‑dose CT with their doctor.
Does obesity affect the effectiveness of RCC treatments?
Obese patients may experience higher rates of side‑effects from targeted therapies, but dose adjustments and supportive care can maintain efficacy. Immunotherapy outcomes appear similar across BMI groups.
Understanding the link between excess weight and kidney cancer empowers you to make informed choices. By keeping an eye on your BMI, adopting a balanced diet, and staying proactive with medical check‑ups, you can dramatically lower the chance that obesity will push a kidney tumor into its most dangerous stage.




Lexi Benson
October 5, 2025 AT 13:11Wow, who knew BMI calculators could double as life coaches?
Vera REA
October 10, 2025 AT 10:11The calculator’s reliance on BMI aligns with multiple cohort studies linking excess adiposity to renal cell carcinoma. Epidemiological data from the Nurses' Health Study and EPIC consistently show an odds ratio above 1.5 for obese individuals. Moreover, the tool correctly flags additional risk factors such as family history and smoking, which are independent predictors of advanced disease. While BMI is an imperfect proxy for body composition, it remains the most feasible metric for large‑scale screening. Overall, the risk estimate provides a useful starting point for patient‑doctor conversations.
John Moore
October 15, 2025 AT 07:11Exactly, the integration of these variables makes the model more robust than a simple weight check. Obesity’s influence on insulin and IGF‑1 pathways is well‑documented, and the calculator highlights that mechanistic link. Adding smoking status captures another major carcinogen that synergizes with metabolic dysfunction. Family history inclusion acknowledges the genetic predisposition many overlook. It’s also worth noting that the calculator’s age threshold helps identify those who might benefit from earlier imaging. In practice, this tool can push clinicians toward proactive monitoring rather than reactive treatment.
Adam Craddock
October 20, 2025 AT 04:11The pathophysiology behind obesity‑driven RCC involves a complex interplay of hormonal and inflammatory signals. Elevated insulin and IGF‑1 promote cellular proliferation while inhibiting apoptosis in renal tubular cells. Chronic low‑grade inflammation, mediated by cytokines such as IL‑6 and TNF‑α, creates a microenvironment conducive to tumor growth. Adipokine dysregulation, particularly increased leptin and reduced adiponectin, further enhances angiogenesis. Lipid accumulation within the kidney can induce oxidative stress, leading to DNA damage and mutagenesis. Understanding these mechanisms underscores why weight management is a critical component of RCC prevention.
Kimberly Dierkhising
October 25, 2025 AT 01:11Obesity acts as a systemic amplifier of oncogenic signaling pathways, a fact repeatedly demonstrated across diverse populations. In the context of RCC, excess adipose tissue raises circulating insulin levels, which in turn stimulate the insulin‑like growth factor‑1 (IGF‑1) cascade, a potent driver of renal tubular cell proliferation. Simultaneously, chronic inflammation emanating from hypertrophic adipocytes releases interleukin‑6, tumor necrosis factor‑alpha, and C‑reactive protein, which collectively induce DNA damage and foster a pro‑tumor microenvironment. Leptin, frequently elevated in obese individuals, exerts pro‑angiogenic effects by up‑regulating vascular endothelial growth factor (VEGF), thereby supplying nascent tumors with essential blood flow. Conversely, adiponectin-generally protective against malignancy-is markedly reduced, stripping renal cells of its anti‑inflammatory and anti‑proliferative benefits. These hormonal imbalances are compounded by lipid infiltration into renal parenchyma, a phenomenon known as renal steatosis, which generates oxidative stress and mitochondrial dysfunction. Oxidative stress precipitates mutagenic events, including point mutations and chromosomal instability, that lay the groundwork for malignant transformation. Epidemiological evidence reinforces this biological narrative; meta‑analyses spanning over one million participants report odds ratios ranging from 1.5 to 2.5 for RCC among those with a BMI ≥ 30 kg/m². Notably, the association strengthens for advanced stage disease, with several studies citing an odds ratio approaching 2.5 for stage III‑IV RCC in obese cohorts. Geographically, the risk elevation persists across continents, appearing in North American, European, and Asian cohorts despite variations in diet and lifestyle. Importantly, the risk is not solely attributable to BMI; waist‑to‑hip ratio and visceral fat volume often correlate even more tightly with RCC incidence. This suggests that central adiposity, rather than overall body mass, may be the critical driver of the observed oncogenic potential. From a clinical perspective, these insights translate into actionable recommendations: regular monitoring of BMI, targeted lifestyle interventions, and vigilant screening for high‑risk individuals. Early detection through imaging modalities such as low‑dose CT can dramatically improve survival outcomes for patients identified before metastatic spread. Ultimately, integrating metabolic health into oncologic risk assessments offers a pragmatic avenue to curb the rising burden of advanced RCC worldwide.
Rich Martin
October 29, 2025 AT 21:11So yeah, shedding a few pounds isn’t just about looking good-it actually flips some of those nasty cancer‑promoting switches off. Even a modest 5‑10% weight loss can bring insulin and inflammation down to healthier levels. Bottom line: a healthier you equals a lower RCC risk.
Buddy Sloan
November 3, 2025 AT 18:11Totally agree, those lifestyle tweaks can make a huge difference! Keep it up, and your kidneys will thank you later :)
SHIVA DALAI
November 8, 2025 AT 15:11The somber reality of renal cell carcinoma looms larger when intertwined with the scourge of obesity, a relationship substantiated by rigorous scientific inquiry. The statistical weight of this association, often quantified as a two‑fold increase, cannot be dismissed as mere coincidence. In the theatre of disease, the obese individual assumes a perilous role, predisposed to advanced pathological stages. It is incumbent upon the medical community to illuminate this peril and champion preventive measures.
Vikas Kale
November 13, 2025 AT 12:11From a translational oncology standpoint, the adipose‑derived cytokine milieu orchestrates a protumorigenic niche via NF‑κB activation and downstream angiogenic cascades. Concurrently, hyperinsulinemia amplifies PI3K/AKT signaling, further destabilizing renal epithelial homeostasis. Epidemiologic cohorts across heterogeneous populations have corroborated a dose‑response curve linking BMI increments to RCC odds ratios upward of 2.0. Thus, integrating metabolic profiling into risk stratification algorithms is both scientifically sound and clinically prudent. The calculator encapsulates these multifactorial inputs, rendering a pragmatic risk estimate for end‑users.
Deidra Moran
November 18, 2025 AT 09:11One has to wonder whether the pharmaceutical giants are quietly capitalizing on the obesity epidemic to inflate RCC treatment sales. The data, though presented with academic veneer, often omits the confounding socioeconomic variables that skew the true risk. Moreover, the reliance on BMI as a surrogate for adiposity feels like a convenient simplification designed to keep the narrative tidy. It’s as if the lurking agenda is to pathologize everyday bodies and expand the market for costly interventions. We must stay vigilant and demand transparency in how these risk tools are crafted and promoted.
Zuber Zuberkhan
November 23, 2025 AT 06:11Let’s keep the conversation hopeful-knowledge is power, and understanding the link between weight and RCC opens doors for proactive health choices. Simple steps like regular exercise and balanced nutrition can shift the odds in our favor. Sharing the calculator empowers individuals to take charge and discuss personalized strategies with their doctors. Together, we can turn statistics into stories of prevention.
Tara Newen
November 28, 2025 AT 03:11The data is crystal clear: obesity dramatically raises RCC risk, and anyone ignoring this fact is doing a disservice to themselves. It’s baffling how some still dismiss lifestyle factors in favor of vague genetic excuses. Wake up and own your health decisions.
Amanda Devik
December 3, 2025 AT 00:11You’ve got this. Small changes add up and every healthy habit is a win. Keep moving forward.
Mr. Zadé Moore
December 7, 2025 AT 21:11Obesity fuels RCC like gasoline to a fire. Extinguish it with smart choices.
Brooke Bevins
December 12, 2025 AT 18:11I’ve seen patients turn their lives around after losing weight, and their cancer outcomes improve dramatically. It’s never too late to start. Your health journey matters, and you’ve got a community cheering you on 😊
Vandita Shukla
December 17, 2025 AT 15:11Actually, the BMI calculator oversimplifies the complex interplay of visceral fat, subcutaneous fat, and ectopic lipid deposition. Advanced imaging studies have shown that individuals with the same BMI can have vastly different renal fat infiltration, which directly impacts oncogenic risk. Moreover, the tool fails to account for sarcopenic obesity, a condition where muscle loss masks high adiposity, further confounding risk assessments. To truly gauge RCC susceptibility, one must incorporate bioelectrical impedance analysis or DEXA scans into the evaluation. Until such multifactorial metrics are standardized, the calculator remains a rough estimate at best.
Susan Hayes
December 22, 2025 AT 12:11Our nation’s healthcare system should prioritize education on obesity and its cancers, protecting citizens from preventable deaths. The data shows that communities with strong public health initiatives see lower RCC rates. Investing in preventive programs is a patriotic duty that saves lives and resources. Let’s champion policies that empower every American to maintain a healthy weight.