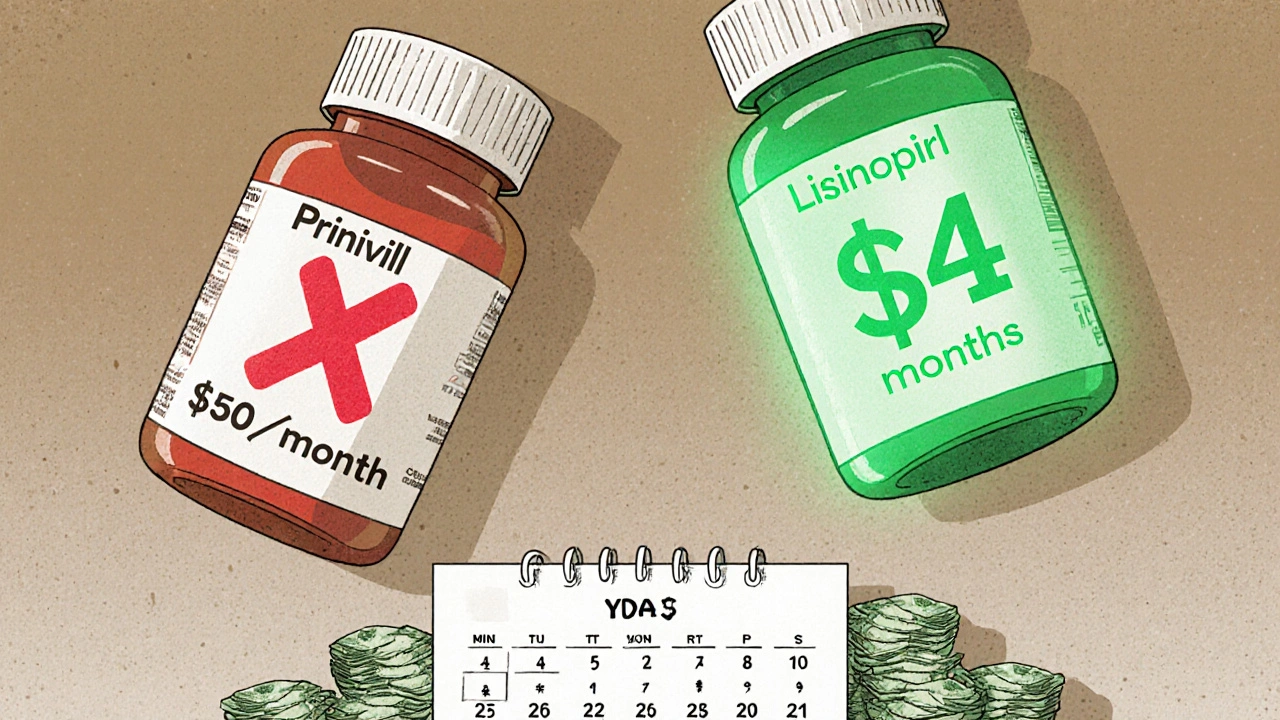
Imagine paying $4 a month for your blood pressure medicine instead of $50. That’s not a dream-it’s what happens when you switch to a generic. For people managing chronic conditions like diabetes, high cholesterol, or asthma, this isn’t just a small saving. It’s a lifetime savings that can add up to tens of thousands of dollars over decades.
Why Generics Are Just as Good as Brand Names
Many people think generics are cheaper because they’re weaker or made with lower-quality ingredients. That’s not true. The U.S. Food and Drug Administration (FDA) requires every generic drug to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in the body-bioequivalence. That means the drug gets into your bloodstream at the same rate and amount as the brand. The FDA’s standard? Within 80-125% of the brand’s performance. That’s tight enough to guarantee identical results. You won’t notice a difference in how it works. A person taking generic lisinopril for hypertension won’t feel any different than someone on Prinivil. The only real difference? The price. And the color of the pill. Or the shape. Those are just inactive ingredients-fillers, dyes, coatings-that don’t affect how the medicine treats your condition.The Real Cost Difference: Numbers That Matter
Let’s break it down with real numbers. A typical brand-name blood pressure pill like Prinivil costs $40-$50 a month. The generic, lisinopril, costs about $4. That’s a 90% drop. For someone taking it for 20 years? That’s $9,000 to $10,000 saved-just on one medication. Same with metformin for type 2 diabetes. Brand-name Glucophage? Around $150 a month. Generic metformin? $5-$10. That’s $1,500-$1,800 saved every year. Over 30 years? More than $50,000. And that’s not even counting other meds-most people with chronic conditions take two or three. Combine them, and the lifetime savings can easily top $100,000. Even more striking: in 2020, generics made up 90% of all prescriptions filled in the U.S., but only 18% of total drug spending. That means 9 out of 10 pills sold were generics, but they accounted for less than 1 in 5 dollars spent on medicine. The rest? Brand-name drugs, priced way higher even though they do the exact same thing.How Savings Lead to Better Health
Money isn’t just about what’s in your wallet-it’s about whether you can afford to take your medicine every day. Studies show that when people can’t pay for their prescriptions, they skip doses, cut pills in half, or stop altogether. The CDC found that 25% of rural patients admitted to skipping meds because of cost. That’s dangerous. Switching to generics changes that. Patients on generics are 18-22% more likely to stick with their treatment long-term. Why? Because they can afford it. Better adherence means fewer hospital visits, fewer complications, and lower overall healthcare costs. One study showed that patients using generics for chronic conditions had 20-30% fewer emergency room trips and hospital stays. That’s not just saving money-it’s saving lives. In countries like Brazil and India, where generic drugs are widely used for HIV, diabetes, and hypertension, treatment adherence jumped by 40%, and death rates dropped by 25% over a decade. This isn’t theory. It’s real-world proof that affordability saves lives.
What’s Holding People Back?
If generics are safe, effective, and cheap, why aren’t more people using them? A big reason? Misinformation. Many still believe generics are “second-rate.” Pharmacists and doctors hear this all the time: “My cousin took a generic and it didn’t work.” But in most cases, it’s not the drug-it’s the placebo effect, or a change in inactive ingredients causing minor side effects like stomach upset. These don’t mean the drug isn’t working. They’re usually temporary and can be solved by switching to a different generic brand. Another barrier? Insurance. Some plans still push brand-name drugs first, even when generics are available. Or they make patients pay more out-of-pocket for generics if they’re not on the preferred list. That’s changing, though. Medicare Part D now covers Medication Therapy Management (MTM) programs, where pharmacists review your whole regimen and help you switch to cheaper, equally effective options. These programs have been shown to cut out-of-pocket costs by 25-35% and improve adherence by 15-25%.How to Maximize Your Lifetime Savings
You don’t need to wait for your doctor to suggest it. Take control:- Ask your pharmacist: “Is there a generic version of this?” Even if your doctor prescribed the brand, the pharmacist can often switch it unless the doctor says no.
- Check the FDA’s Orange Book online-it lists approved generics and their brand equivalents. No need to pay for it; it’s free.
- Use mail-order pharmacies or bulk discount programs. Many generics cost under $10 for a 90-day supply through Walmart, Costco, or GoodRx.
- Sign up for Medicare Part D’s MTM program if you’re eligible. It’s free, and a pharmacist will review all your meds and find savings.
- Don’t assume your insurance will automatically choose the cheapest option. Always double-check your copay before filling a prescription.
The Bigger Picture: Generics Are Changing Healthcare
The U.S. spent $350 billion on prescription drugs in 2020. Generics saved $338 billion that year alone. Over the past decade, they’ve saved the system nearly $2.4 trillion. That’s not just a win for patients-it’s a win for the whole healthcare system. And it’s only getting bigger. Around $150 billion in brand-name drug sales will lose patent protection between 2023 and 2027. That means more generics hitting the market. Newer complex generics-like inhalers, injectables, and combination pills-are also becoming more common, making it possible to replace even the most expensive chronic disease treatments. The Inflation Reduction Act of 2022 capped insulin costs at $35 a month for Medicare patients. While that’s a start, generics make that cap even more powerful. If your insulin is already generic, you’re paying $5-$15 a month instead of $35. That’s real relief.What’s Next? Biosimilars and Beyond
The next wave? Biosimilars. These are generic versions of biologic drugs-complex medicines made from living cells, used for conditions like rheumatoid arthritis, Crohn’s disease, and some cancers. They’re harder to copy than regular pills, but they’re here now. And they’re already cutting costs by 15-35%. IQVIA predicts biosimilars will save the U.S. healthcare system $300 billion over the next decade. That’s on top of the $2.4 trillion saved by traditional generics. This isn’t the end of the story-it’s the next chapter.Final Thought: Your Health Is Worth the Switch
Chronic conditions aren’t temporary. They last decades. And every month you pay full price for a brand-name drug, you’re throwing away money you could be using for food, rent, or savings. Generics don’t just lower your monthly bill-they lower your lifetime risk of complications, hospital stays, and early death. There’s no downside. No trade-off. No compromise. Just a smarter, simpler way to stay healthy without breaking the bank.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. That means they work the same way in your body. Thousands of studies confirm they’re equally effective for treating chronic conditions like high blood pressure, diabetes, and asthma.
Why do generics cost so much less?
Brand-name companies spend billions on research, clinical trials, and marketing. Generics don’t need to repeat those expensive steps-they just prove they work the same way. That cuts their costs dramatically. Manufacturers can sell them for 80-85% less and still make a profit.
Can I switch from my brand-name drug to a generic without talking to my doctor?
In most cases, yes. Pharmacists can legally substitute a generic unless the prescription says “Dispense As Written” or “No Substitution.” Always ask your pharmacist first-they can check your prescription and make the switch if allowed. If they can’t, they’ll tell you how to get your doctor to approve it.
What if I feel different after switching to a generic?
Sometimes, changes in inactive ingredients (like fillers or dyes) can cause minor side effects like nausea or headaches. These are usually temporary and go away after a few days. If they don’t, talk to your pharmacist. They can switch you to a different generic brand-there are often multiple manufacturers for the same drug.
Do insurance plans cover generics?
Yes, and they usually cover them better than brand-name drugs. Most insurance plans have lower copays for generics. Some even require you to try the generic first before covering the brand. Medicare Part D and many private plans now include Medication Therapy Management programs that help you find the cheapest, most effective options.
Are there any chronic conditions where generics aren’t available?
Most common chronic conditions have generics available-hypertension, diabetes, high cholesterol, asthma, depression, and thyroid disorders. Some newer or very complex drugs (like certain biologics for autoimmune diseases) still don’t have generics, but biosimilars are becoming more common. Always check with your pharmacist or use the FDA’s Orange Book to see what’s available.



Kihya Beitz
November 14, 2025 AT 17:21Wow, so the government just magically made all these drugs cheaper? Next they’ll tell me my WiFi is free too. 😒
Meanwhile, my insurance still charges me $20 for lisinopril because ‘it’s not on the preferred list’ - guess the ‘savings’ only apply to people who can navigate bureaucracy like a ninja.
Jennifer Walton
November 16, 2025 AT 02:44Cost is not the same as value. The body does not care about price tags. It responds to chemistry. And chemistry, in this case, is identical.
Yet we cling to branding like it’s a spiritual truth.
BABA SABKA
November 17, 2025 AT 18:50Y’all in the US act like generics are some kind of socialist conspiracy. In Nigeria, we take generics because we have no choice - and guess what? We’re not dropping dead. We’re managing. The FDA standards? Solid. The pricing? Criminal. But the science? Unimpeachable.
Stop treating your medication like a luxury brand and start treating it like medicine.
Chris Bryan
November 19, 2025 AT 15:42Who funds the generic manufacturers? Big Pharma subsidiaries. The FDA? Regulated by the same lobbyists. This is all a trap - they want you to think you’re saving money while they just repackage the same poison at a discount.
They’re not saving you. They’re conditioning you to accept less.
Jonathan Dobey
November 20, 2025 AT 07:12Let’s be real - we live in a society where a pill with a different dye is treated like a betrayal of the soul.
Brand-name drugs are the opium of the middle class - a placebo for identity, not physiology.
Generics are the truth serum of capitalism: if it works, why pay more? Because we’ve been trained to equate cost with worth.
And that’s not economics - that’s pathology.
ASHISH TURAN
November 21, 2025 AT 00:44In India, generics are the backbone of public health. My grandfather took metformin for 25 years - generic, from a small pharma in Hyderabad. Lived to 89. No hospitalizations. No drama.
It’s not magic. It’s math. And math doesn’t lie.
Ryan Airey
November 21, 2025 AT 03:34People still think generics are ‘inferior’? That’s not ignorance - that’s willful stupidity.
You want to die because you’re too lazy to check if your prescription has a generic? Fine. But don’t act surprised when your kidneys fail.
Pharmacists aren’t there to hold your hand. They’re there to save your life. Use them.
Hollis Hollywood
November 22, 2025 AT 04:05I just want to say - I used to be one of those people who refused generics because I was scared something would go wrong.
Then I switched to generic atorvastatin after my pharmacist explained the bioequivalence data. No side effects. My cholesterol dropped the same.
It took me six months to get over the psychological barrier - not because the drug was different, but because I’d been conditioned to fear the word ‘generic.’
It’s not about the pill. It’s about trust. And trust, in this case, was misplaced.
Now I tell everyone. Not because I’m an activist - because I don’t want anyone to waste money like I did.
Aidan McCord-Amasis
November 23, 2025 AT 08:47Generics = 💰🔥
Brand names = 🤑💸
Stop being a sucker.
Adam Dille
November 24, 2025 AT 01:26My mom switched to generic insulin last year - went from $130/month to $12 with GoodRx.
She cried. Not because she was sad - because she finally felt like she could breathe again.
It’s not just about pills. It’s about dignity.
Thanks for writing this. I’m sharing it with everyone I know.
Katie Baker
November 24, 2025 AT 05:08YES. I switched to generic metformin last month and my copay dropped from $55 to $3. I almost didn’t believe it.
And I felt the same - no weird side effects, no crash, no ‘it’s not working’ vibes.
Why do we make this so hard? It’s literally the same drug.
Everyone should do this. Seriously.
John Foster
November 25, 2025 AT 19:17There is a deeper metaphysical question here: if a drug performs identically but lacks the branding, does it still carry the weight of legitimacy in a consumerist society?
Our attachment to brand names is not rational - it is ritualistic. We don’t trust the science; we trust the logo.
Generics expose the hollowness of pharmaceutical capitalism - not because they are inferior, but because they reveal how little the medicine itself matters, compared to the myth we’ve constructed around it.
And that myth? It’s killing us - slowly, quietly, with interest payments.
Edward Ward
November 26, 2025 AT 16:45I’ve spent years researching this - checking the FDA’s Orange Book, cross-referencing bioequivalence studies, talking to pharmacists in three states, even calling generic manufacturers directly.
And here’s what I’ve found: the only difference between brand and generic is the label.
Same active ingredient. Same dissolution rate. Same clinical outcomes. Same safety profile.
Even the inactive ingredients? Often identical - or at least within FDA tolerance thresholds that ensure no meaningful difference.
So why do we still pay more?
Because we’ve been lied to for decades - by marketing, by fear, by doctors who never bothered to educate us.
It’s not about the drugs.
It’s about the system.
And the system is rigged.
But you? You can opt out.
Just ask.
Just check.
Just switch.
It’s not radical.
It’s just smart.