After a heart attack, bypass surgery, or other major cardiac event, the last thing you want to do is sit still. But jumping back into your old routine? That can be just as dangerous. The truth is, exercise isn't just okay after a heart event-it’s one of the most powerful tools you have to rebuild your health. The right kind of movement, done at the right time and intensity, can cut your risk of another cardiac event by up to 30%. Yet, most people don’t know how to start safely. This isn’t about pushing hard. It’s about rebuilding smart.
Phase 1: Starting Slow in the Hospital
Your rehab begins before you even leave the hospital. During this acute phase, your body is healing, and your heart is fragile. The goal isn’t fitness-it’s circulation. Simple movements like ankle pumps (flexing your feet up and down while lying down) and seated marching (lifting your knees gently while sitting) are all you need. These exercises help prevent blood clots and keep your circulation moving without raising your heart rate too much. Most patients are cleared for 1-2 minutes of activity at a time, with rest in between. You might feel tired after walking from your bed to the bathroom-and that’s normal. Your heart is working hard to heal. Don’t push. Don’t rush. Just move.
Phase 2: Building Strength After Discharge
Once you’re home, you enter the early outpatient phase. This is where real progress begins, but only if you follow a clear plan. Start with walking. Five to ten minutes a day, five days a week. That’s it. No need to go fast or far. Use the talk test: if you can speak in full sentences without gasping, you’re in the right zone. Your target heart rate should be your resting heart rate plus 20 to 30 beats per minute. If you’re on beta-blockers-which most people are after a heart event-your max heart rate might be 20-30% lower than before. That’s not a problem. It’s expected. Your doctor or rehab specialist will adjust your targets accordingly.
At this stage, you’re also adding light strength training. Use resistance bands or light dumbbells (1-3 pounds) for seated arm curls or shoulder raises. Two days a week is enough. Focus on control, not weight. One study found that patients who did even minimal strength training had better balance, less fatigue, and improved daily function within just six weeks. The key is consistency, not intensity.
Phase 3: Long-Term Maintenance
After 6 to 12 weeks, you move into the maintenance phase. This is where you aim for the American Heart Association’s standard: at least 150 minutes of moderate exercise per week. That breaks down to 30 minutes, five days a week. You can split it into two 15-minute walks if that’s easier. The type of exercise matters less than the habit. Walking, cycling on a stationary bike, swimming, or even dancing around your living room-all count. The goal is to get your heart rate up enough that you’re breathing harder but still able to talk. Avoid anything that causes chest pressure, dizziness, or sudden shortness of breath. If you feel any of those, stop immediately.
Also, add muscle-strengthening activities twice a week. Bodyweight squats, wall push-ups, or lifting groceries can all count. You don’t need a gym. You just need to move regularly. People who stick with this routine for a year are 47% less likely to be readmitted to the hospital. That’s not a small number. That’s life-changing.

Supervised Rehab vs. Going It Alone
You might think, “I can just follow a general fitness plan.” But here’s the catch: cardiac rehab programs aren’t just about exercise. They’re about safety, education, and support. Patients in formal programs recover 25% faster and have 30% lower five-year death rates than those who try to manage on their own. Why? Because supervised programs use real-time monitoring. Your heart rate, blood pressure, and symptoms are tracked while you move. If something goes wrong, someone’s right there. In one study, 27% of people exercising without supervision pushed themselves too hard in the first month-enough to trigger chest pain or abnormal heart rhythms.
Supervised rehab also teaches you how to listen to your body. You learn the seven warning signs that mean you need to stop: chest pain, pain in your arm or jaw, dizziness, palpitations, unusual shortness of breath, slurred speech, or sudden weakness. Most people don’t know these until they’re taught. And you’re not just learning exercise-you’re learning nutrition, stress management, and how to take your meds correctly. All of it works together.
What’s New in 2026?
Cardiac rehab has evolved. In 2023, the American Heart Association updated its guidelines to say low-risk patients can start walking within 24 hours after a procedure-down from 48 hours. Research shows this leads to 19% faster recovery. Also, high-intensity interval training (HIIT) is now proven safe for stable patients. Short bursts of faster walking or cycling, followed by rest, can improve heart function more than steady, slow exercise. But this isn’t for everyone. Only those cleared by their doctor and who’ve completed the first two phases should even consider it.
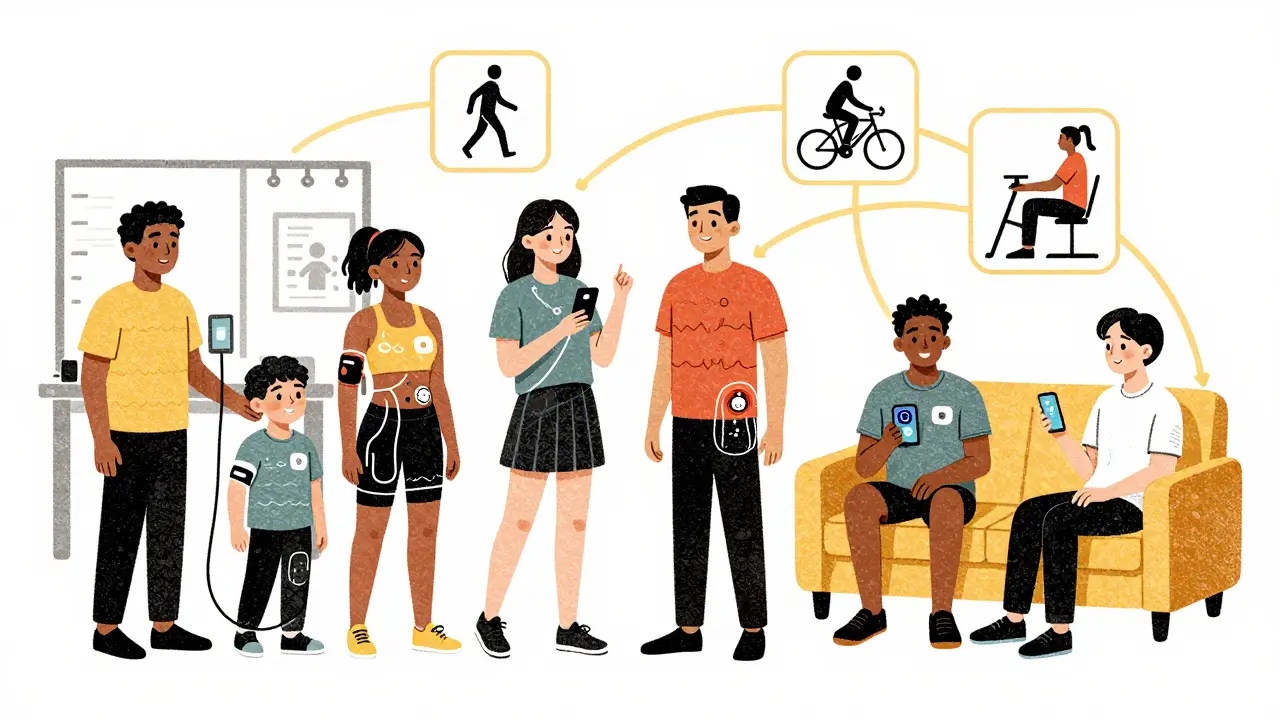
Technology is helping too. Many programs now use Bluetooth heart rate monitors and ECG patches you wear at home. These send real-time data to your rehab team. If your heart rate spikes unexpectedly, they get an alert. In 2024, the Cleveland Clinic launched a hybrid program combining 12 in-person sessions with 24 virtual ones-using FDA-cleared wearables. This has boosted participation, especially for people who can’t drive or work full-time.
Common Mistakes and How to Avoid Them
- Mistake: Skipping the first phase and jumping into walking too fast. Solution: Wait for your doctor’s green light. Even if you feel fine, your heart is still healing.
- Mistake: Ignoring medication effects. Beta-blockers lower your heart rate. If you’re using old fitness targets, you might think you’re not working hard enough. Solution: Use the talk test and RPE (Rating of Perceived Exertion) scale instead. Aim for 11-14 on the 6-20 scale-meaning you feel light to somewhat hard effort.
- Mistake: Exercising in extreme heat or cold. Your heart works harder in those conditions. Solution: Move indoors. Mall walking, home workouts, or using a stationary bike in your garage are great alternatives.
- Mistake: Not tracking symptoms. Solution: Keep a simple journal. Note how you felt before, during, and after each session. Over time, you’ll spot patterns-like if you feel tired after eating a heavy meal or if your meds make you dizzy at certain times.
Why So Few People Join Rehab
Even though cardiac rehab saves lives, only about 30-40% of eligible patients enroll. The reasons? Transportation is a big one. If you don’t drive or live far from a clinic, it’s hard to get there. Work schedules, cost concerns, and lack of awareness also play a role. Some people think, “I’m not sick anymore, so I don’t need it.” But rehab isn’t for being sick-it’s for staying well. Medicare covers 36 sessions, and many private insurers follow suit. If your doctor didn’t mention it, ask. You have the right to be referred.
And if you can’t get to a clinic, hybrid programs are now widely available. Virtual sessions with a certified exercise physiologist, combined with wearable tech, can give you the same safety net as in-person rehab. You’re not alone in this. Thousands are doing it remotely-and doing well.
Real Talk: What Patients Say
One woman from Brisbane, 68, had a stent placed after a mild heart attack. She was terrified to walk more than 10 minutes. After eight weeks in a supervised program, she started walking her neighborhood loop daily. “I used to think exercise would kill me,” she said. “Now I know it’s the thing keeping me alive.”
Another man, 72, skipped rehab because he thought it was “for old people.” He tried walking on his own. Two weeks later, he had chest pain and ended up in the ER. His doctor told him he’d pushed too hard. He enrolled in rehab after that. “I learned how to listen to my body,” he said. “That’s the biggest gift.”
Can I start exercising the same day I leave the hospital?
It depends on your condition. For low-risk patients, gentle movement like ankle pumps or short walks may begin within 24 hours. But you should only do this under the direct guidance of your medical team. Never start walking or lifting on your own without clearance. Even if you feel fine, your heart is still healing.
How do I know if I’m exercising too hard?
Use the talk test: if you can’t speak in full sentences without gasping, you’re going too hard. Also watch for warning signs: chest pain, dizziness, unusual shortness of breath, palpitations, or pain radiating to your arm or jaw. If any of these happen, stop immediately and rest. If symptoms don’t go away in a few minutes, call your doctor.
Do I need to join a formal cardiac rehab program?
You don’t absolutely need it, but it’s the safest and most effective way to restart. Formal programs monitor your heart, teach you warning signs, adjust for your meds, and reduce your risk of another event by up to 30%. If you can’t attend in person, hybrid programs with virtual coaching and wearable tech are now widely available and just as effective.
What if I’m on beta-blockers? Can I still exercise?
Yes, and you should. Beta-blockers lower your heart rate, so your target heart rate will be lower than before your event. Don’t try to match your old fitness levels. Use the talk test and RPE scale instead. Your rehab team will adjust your goals based on your meds. Exercising while on beta-blockers is not only safe-it’s essential for long-term recovery.
How long until I feel normal again?
Most people notice improved energy and less fatigue within 4 to 6 weeks of starting a consistent routine. Full recovery-where you can do daily activities without worry-usually takes 3 to 6 months. But everyone heals differently. Focus on progress, not perfection. Even small increases in activity, done safely, build up over time.
Is high-intensity exercise safe after a heart event?
For some patients, yes-but only after completing the first two phases of rehab and getting approval from your doctor. Studies show high-intensity interval training (HIIT) can improve heart function more than steady exercise. But it’s not for everyone. If you’re still in the early recovery phase or have other health issues, stick to moderate activity. Never jump into HIIT on your own.
Next Steps
If you’ve had a heart event and haven’t been referred to cardiac rehab, ask your doctor today. If you’re already in a program, keep showing up-even on days you don’t feel like it. The real win isn’t how fast you walk or how much weight you lift. It’s that you’re alive, moving, and taking control. That’s not just recovery. That’s renewal.





