Hyperkalemia Risk Assessment Tool
Personal Risk Assessment
This tool helps you understand your risk of developing dangerous hyperkalemia while taking medications for heart, blood pressure, or kidney conditions. Results are for informational purposes only and should not replace professional medical advice.
Your Risk Assessment
Risk Score (0-10)
Key Risk Factors
When Your Heart Is at Risk from Common Medications
You’re taking blood pressure medicine because your doctor told you it saves lives. You’re on a pill for heart failure or kidney disease because it slows damage. But what if that same pill is quietly raising your potassium to dangerous levels-levels that can stop your heart?
It’s not rare. It’s not unusual. In fact, hyperkalemia-high potassium in the blood-is one of the most under-recognized drug side effects in modern medicine. And it’s not just a lab number. At levels above 5.5 mEq/L, it starts messing with your heart’s rhythm. Above 6.5 mEq/L, it can trigger sudden cardiac arrest. And it’s often caused by the very drugs meant to protect you.
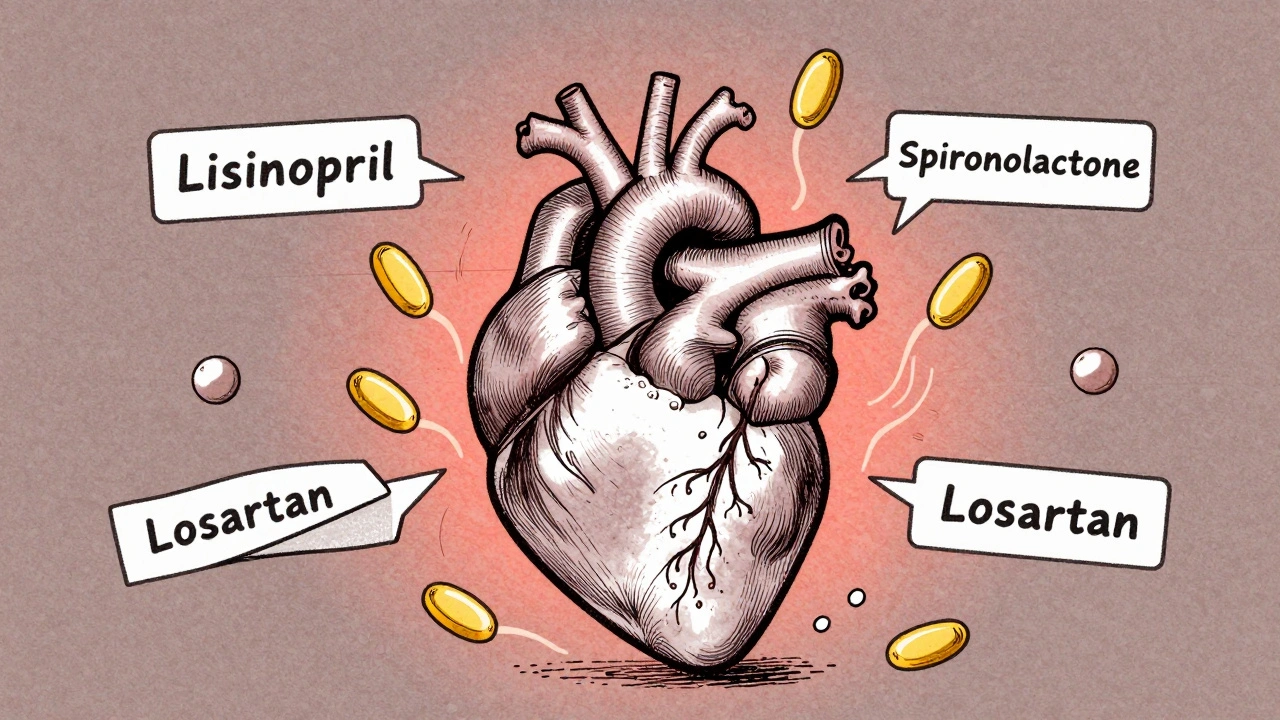
How Medications Turn Potassium Into a Time Bomb
Potassium is essential. It helps your muscles contract, including your heart. But too much, and your heart cells can’t reset properly between beats. That’s when arrhythmias start. The problem isn’t your diet-it’s your meds.
The biggest culprits are drugs that block the renin-angiotensin-aldosterone system (RAASi). That’s a mouthful, but it’s just a fancy name for a group of drugs that include:
- ACE inhibitors like lisinopril
- ARBs like losartan
- Mineralocorticoid antagonists like spironolactone
- Direct renin inhibitors like aliskiren
These drugs are lifesavers for people with high blood pressure, heart failure, or chronic kidney disease. But they reduce aldosterone, the hormone that tells your kidneys to flush out potassium. So potassium builds up. And in people with kidney problems, diabetes, or over 65, it builds up fast.
Worse? Combining spironolactone with an ACE inhibitor and an antibiotic like trimethoprim-sulfamethoxazole can make your risk of sudden death 5.5 times higher than using spironolactone alone.
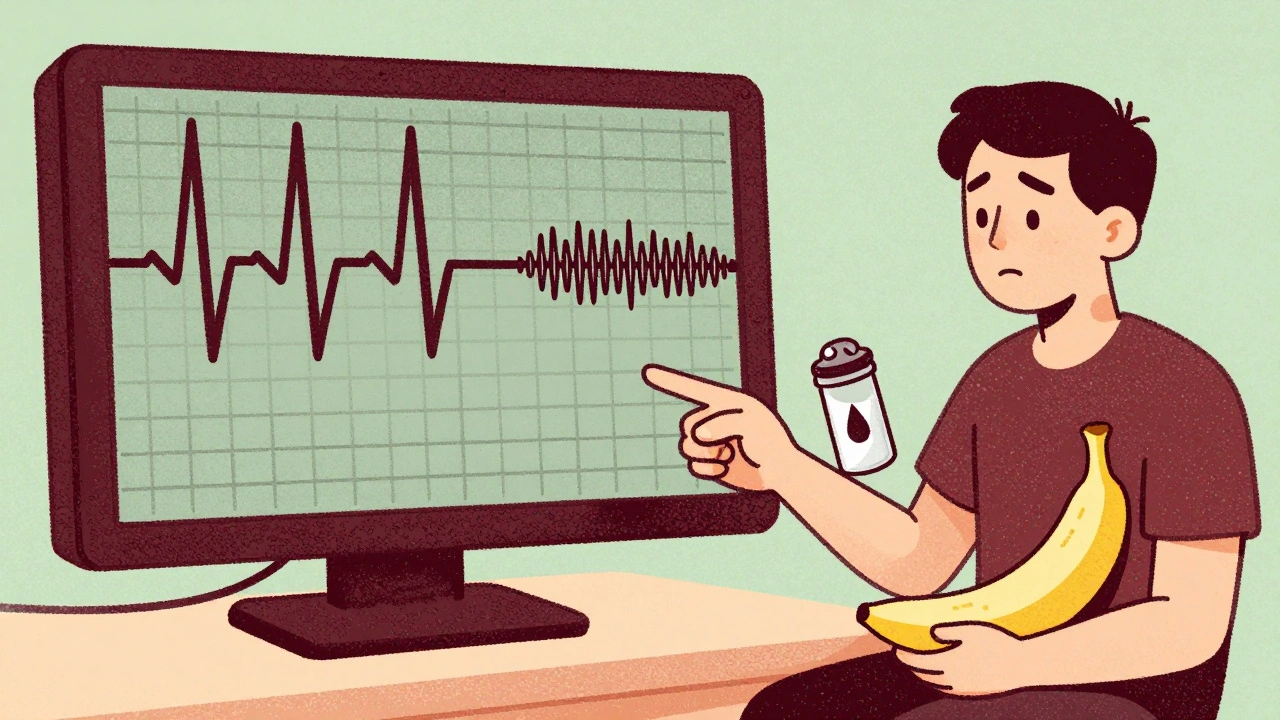
What Happens When Potassium Hits 6.5 or Higher
At 5.5 mEq/L, you might feel nothing. No dizziness. No chest pain. Just a quiet, creeping danger.
But by the time potassium hits 6.5 mEq/L or more, your heart’s electrical system starts to unravel. You’ll see it on an ECG:
- Peaked T-waves (the first warning sign)
- Widened QRS complex (your heart’s signal is slowing)
- Prolonged PR interval (delayed communication between chambers)
- Sine wave pattern (a pre-arrest rhythm)
These aren’t just lines on a graph. They’re signs your heart is about to go into ventricular fibrillation-where it quivers instead of pumps. That’s when you collapse. That’s when you die.
And here’s the cruel part: many people don’t feel anything until it’s too late. The Cleveland Clinic says symptoms, if they appear, are vague-muscle weakness, fatigue, nausea. Easy to ignore. Easy to mistake for aging or stress.
Why Doctors Are Stuck Between a Rock and a Hard Place
Here’s the real dilemma: stopping RAASi drugs reduces potassium, but it also increases your risk of heart attack, stroke, and death from heart failure. A 2015 study found that 38% of patients had their RAASi medication lowered or stopped just because of mild hyperkalemia-even though those drugs were keeping their hearts alive.
For years, the only solution was to stop the drug. But now we know that’s often the wrong move. Patients who stop RAASi drugs after a hyperkalemia episode have higher long-term mortality. So what’s the answer?
It’s not about avoiding the drug. It’s about managing the side effect.
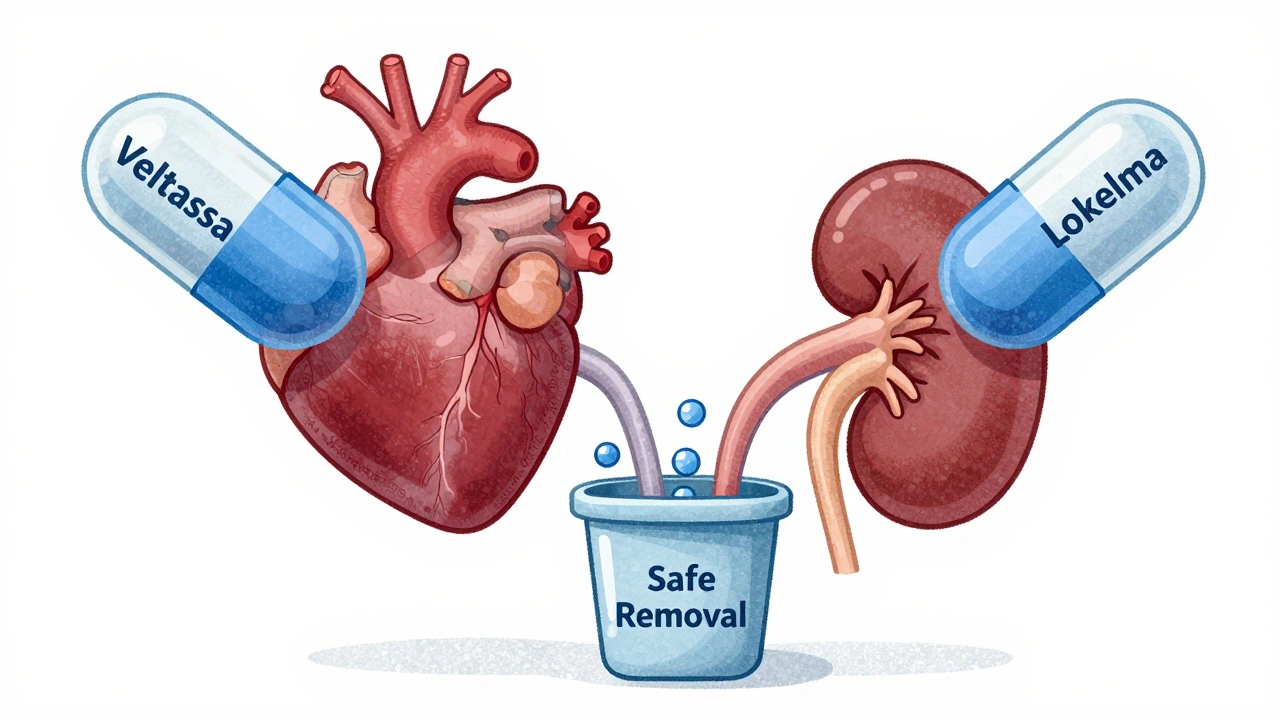
The New Game-Changers: Potassium Binders
Before 2015, we had no good way to keep potassium low without ditching the heart-protecting meds. Then came two breakthroughs:
- Patiromer (Veltassa)-taken daily, binds potassium in the gut and flushes it out.
- Sodium zirconium cyclosilicate (Lokelma)-works fast, lowers potassium within hours.
Studies show these drugs can drop potassium by 0.4 to 1.0 mEq/L. More importantly, they let patients stay on their RAASi meds. One trial found that 86% of patients stayed on their full-dose heart medication when using patiromer, compared to just 66% in the placebo group.
They’re not perfect. About 1 in 5 people get constipation. A smaller number get diarrhea. But compared to the risk of stopping lifesaving drugs? The trade-off is worth it.
What to Do If You’re on RAASi Medications
If you’re taking any of these drugs-especially with kidney disease, diabetes, or over 65-here’s what you need to do:
- Get your potassium checked every 1 to 4 weeks, especially after starting or changing a dose. Don’t wait for symptoms.
- Avoid salt substitutes. Many contain potassium chloride. That’s like pouring fuel on the fire.
- Watch your diet. Limit high-potassium foods: bananas, oranges, potatoes, tomatoes, spinach, beans, and dairy. Aim for under 3,000 mg per day.
- Talk to your doctor before taking new meds. Even over-the-counter drugs like NSAIDs (ibuprofen, naproxen) can raise potassium. So can certain herbal supplements.
- Ask about potassium binders. If your levels creep up, don’t assume you have to stop your heart medication. Ask: “Can we use a binder instead?”
Emergency Treatment: When Seconds Count
If you’re in the hospital with potassium above 6.5 mEq/L and ECG changes, time is everything. Here’s what happens:
- Calcium gluconate is given IV first. It doesn’t lower potassium-but it protects your heart muscle from the electrical chaos. Effects start in under 3 minutes.
- Insulin and glucose are given together. Insulin pushes potassium into your cells. Glucose prevents low blood sugar. This drops potassium by 0.5-1.5 mEq/L in 15-30 minutes.
- Albuterol via nebulizer does the same thing-shifts potassium into cells. Works fast, no IV needed.
- Diuretics or dialysis are used next to remove potassium from the body entirely.
These steps are standard in emergency rooms. But they’re only for acute crises. Long-term, you need a plan.
The Future: Keeping Your Heart Safe Without Sacrificing Your Meds
For decades, hyperkalemia meant stopping the drug. That’s changing. Today’s guidelines from the National Kidney Foundation and the American Heart Association now recommend potassium binders as first-line treatment for patients who need RAASi therapy.
Modeling studies suggest that if we stop discontinuing RAASi drugs due to mild hyperkalemia, we could cut heart-related deaths in high-risk patients by 20-25%. That’s tens of thousands of lives saved every year.
The goal isn’t to avoid potassium. It’s to manage it. Your heart medication isn’t the enemy. Unchecked potassium is.
Frequently Asked Questions
Can high potassium from meds be reversed without stopping my heart medication?
Yes. Potassium binders like patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) are designed to lower potassium without making you stop your RAASi drugs. These are now the standard of care for patients who need ongoing heart or kidney protection.
I have kidney disease. Should I avoid RAASi drugs because of potassium risk?
No. RAASi drugs are the most effective way to slow kidney damage and reduce heart attacks in people with kidney disease. The risk of stopping them is greater than the risk of managing potassium with binders and diet. Work with your doctor to monitor levels and use binders if needed.
What foods should I avoid if I’m at risk for hyperkalemia?
Limit high-potassium foods like bananas, oranges, potatoes, tomatoes, spinach, dried fruit, beans, and salt substitutes. A daily intake under 3,000 mg is generally recommended. You don’t need to eliminate them-just reduce portions and choose lower-potassium alternatives like apples, cabbage, and white rice.
Can I check my potassium level at home?
Not reliably. Home finger-prick tests for potassium are not accurate enough for clinical decisions. Blood tests done in a lab are still the gold standard. If you’re on RAASi meds, schedule regular blood work-don’t wait for symptoms.
Are potassium binders safe for long-term use?
Yes. Both patiromer and sodium zirconium cyclosilicate have been studied for over two years in clinical trials. Side effects like constipation or diarrhea are usually mild and manageable. The long-term benefit-keeping you on life-saving heart and kidney meds-far outweighs the risks.
What should I do if I feel weak or have palpitations while on these meds?
Don’t ignore it. Weakness, irregular heartbeat, or nausea could be early signs of high potassium. Call your doctor right away. If symptoms are sudden and severe-like chest pain or fainting-go to the ER. Hyperkalemia can turn deadly in minutes.
Final Thought: Don’t Let Fear Stop Your Treatment
Medications aren’t perfect. But they’re not the enemy. Hyperkalemia is the silent threat-and it’s preventable. You don’t have to choose between your heart and your potassium. With better monitoring, smarter diet choices, and new binders, you can have both.
Ask questions. Get tested. Know your numbers. Your heart will thank you.



Michael Dioso
December 5, 2025 AT 19:35Lynette Myles
December 6, 2025 AT 21:22Lucy Kavanagh
December 7, 2025 AT 00:31Mark Curry
December 8, 2025 AT 16:13Krishan Patel
December 10, 2025 AT 04:10Carole Nkosi
December 10, 2025 AT 13:42Manish Shankar
December 12, 2025 AT 10:33aditya dixit
December 12, 2025 AT 16:01William Chin
December 13, 2025 AT 11:07Mark Ziegenbein
December 13, 2025 AT 16:11luke newton
December 15, 2025 AT 03:12an mo
December 16, 2025 AT 18:21Chris Brown
December 17, 2025 AT 02:50