When your body stops making insulin, life changes overnight. Type 1 diabetes isn’t caused by poor diet or lack of exercise. It’s an autoimmune condition where your immune system attacks the insulin-producing cells in your pancreas. No one chooses this. No one causes it. But once diagnosed, managing it becomes your new normal - and it’s doable. Millions live full, active lives with type 1 diabetes. The key? Understanding the signs, getting the right diagnosis, and knowing your insulin options.
What Are the Warning Signs of Type 1 Diabetes?
The symptoms don’t sneak up. They hit fast - often over days or weeks. You might notice you’re drinking way more water than usual. You’re peeing every hour, even at night. Despite eating more, you’re losing weight without trying. Your energy is gone. You feel tired all the time, even after sleeping. Your vision gets blurry. Cuts take forever to heal. Your mouth feels dry, no matter how much you drink. These aren’t just inconveniences. They’re your body screaming for help. When insulin is gone, sugar can’t get into your cells for energy. Instead, it builds up in your blood. Your kidneys try to flush it out - that’s the frequent urination. Your body starts breaking down fat for fuel, which creates toxic acids called ketones. That’s how diabetic ketoacidosis (DKA) starts. DKA can develop in less than 24 hours if left untreated. It’s life-threatening. Many people are diagnosed with type 1 diabetes only after ending up in the ER with DKA. Some people, especially adults, may have milder symptoms at first. That’s why it’s often misdiagnosed as the flu or stress. But if you’re losing weight, thirsty all the time, and tired despite eating normally - don’t ignore it. Early detection saves you from hospitalization and long-term damage.How Is Type 1 Diabetes Diagnosed?
Diagnosis isn’t just about feeling unwell. It’s about lab tests that confirm what’s happening inside your body. The first test most doctors use is the A1C test. It measures your average blood sugar over the past 2 to 3 months. If your A1C is 6.5% or higher on two separate tests, you have diabetes. Other tests include:- Fasting plasma glucose: After not eating for 8 hours, a blood sugar level of 126 mg/dL or higher confirms diabetes.
- Random plasma glucose: If your blood sugar is 200 mg/dL or higher and you have symptoms like excessive thirst or urination, that’s a clear sign.
- Oral glucose tolerance test: You drink a sugary solution, and your blood sugar is checked 2 hours later. A result of 200 mg/dL or higher means diabetes.
What Are the Insulin Therapy Options Today?
You can’t survive without insulin. But how you get it has changed dramatically in the last decade. The two main approaches are multiple daily injections (MDI) and insulin pumps. MDI, also called basal-bolus therapy, means you take two types of insulin every day. A long-acting insulin (like glargine or detemir) gives you steady background coverage for 24 hours. Then, before every meal, you inject a rapid-acting insulin (like lispro, aspart, or glulisine) to cover the carbs you eat. You’ll need to count carbs, check your blood sugar 4 to 10 times a day, and adjust doses based on what you eat, how active you are, and your current blood sugar. Insulin pumps are small devices worn on your body that deliver insulin through a tiny tube under your skin. They give you a continuous low dose (basal rate) and let you program extra doses (boluses) for meals. Modern pumps don’t just deliver insulin - they talk to your continuous glucose monitor (CGM). Systems like the Medtronic MiniMed 780G or Tandem t:slim X2 with Control-IQ can automatically adjust insulin delivery based on your glucose levels. If your sugar starts dropping, the pump slows or stops insulin. If it’s rising, it gives a correction dose. This reduces the mental load and lowers your risk of lows and highs. The ADA recommends most people with type 1 diabetes aim for blood sugar levels between 80-130 mg/dL before meals and under 180 mg/dL two hours after eating. Your A1C goal is usually under 7%, but for older adults or those with other health issues, 7.5%-8% may be safer to avoid dangerous lows.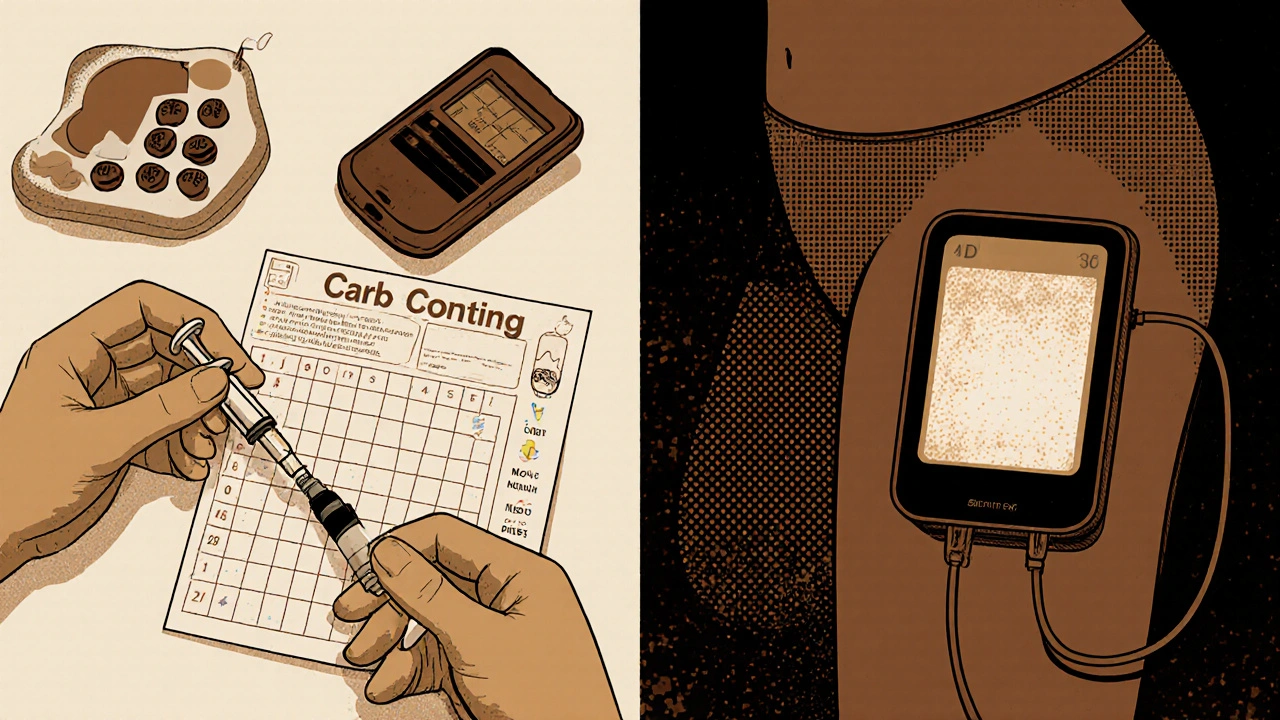
Why Continuous Glucose Monitoring Is a Game-Changer
Before CGMs, people had to prick their fingers 4 to 10 times a day. It was painful, inconvenient, and gave only snapshots of your blood sugar. CGMs use a tiny sensor inserted under your skin that measures glucose in your fluid every 5 minutes. It sends data to your phone or pump in real time. Studies show people using CGMs lower their A1C by 0.5% to 0.8% compared to those using fingersticks. That might sound small, but it cuts your risk of complications by up to 40%. You see trends - not just numbers. You know if your sugar is rising fast after a meal or dropping while you sleep. You get alerts before you feel symptoms. For parents of kids with type 1, CGMs mean fewer nighttime panic checks. Most insurance plans now cover CGMs for type 1 diabetes. The sensors last 7 to 14 days, depending on the brand. You still need to calibrate some models with a fingerstick, but newer ones don’t require it.What Else Do You Need to Manage Type 1 Diabetes?
Insulin isn’t the whole picture. Managing type 1 means a daily routine that includes:- Carb counting: You learn how many grams of carbs your body needs insulin for. Ratios vary - 1 unit per 5 grams for some, 1 unit per 30 grams for others. It’s personal.
- Regular lab tests: Every 3 to 6 months, you get an A1C test. Annually, you check your kidney function, cholesterol, thyroid, and liver. Type 1 diabetes increases your risk for other autoimmune conditions like celiac disease and thyroid disorders.
- Hypoglycemia training: Low blood sugar (below 70 mg/dL) is dangerous. You need to recognize shaking, sweating, confusion, or dizziness. Always carry 15 grams of fast-acting sugar - glucose tablets, juice, or candy. Wait 15 minutes, recheck. Repeat if needed.
- Diabetes education: Most hospitals offer 10 to 20 hours of initial training. You learn injection techniques, carb counting, sick-day rules, and how to handle exercise. Don’t skip this. It’s not optional - it’s survival.

What’s New in Type 1 Diabetes Treatment?
The future is here - and it’s not just about better insulin. In late 2022, the FDA approved teplizumab (Tzield). It’s the first drug that can delay the onset of type 1 diabetes in people at high risk. If you have two or more autoantibodies and your blood sugar is still normal, this 14-day IV treatment can push off clinical diabetes by more than two years on average. It’s not a cure - but it’s a breakthrough. Stem cell therapies are advancing fast. Vertex Pharmaceuticals’ VX-880 treatment uses lab-grown insulin-producing cells from donor stem cells. In early 2023 trials, 89% of participants stopped needing insulin injections after 90 days. This isn’t available to the public yet - but it’s coming. Cost remains a huge barrier. The average annual cost of managing type 1 diabetes is over $20,000. Insulin alone makes up nearly 27% of that. Many people still ration insulin because they can’t afford it. That’s deadly. Advocacy and policy changes are urgently needed.Can Type 1 Diabetes Be Cured?
Not yet. But the goal is shifting from just surviving to thriving. With modern tools - pumps, CGMs, smarter insulin, and emerging therapies - people with type 1 diabetes are living longer, healthier lives than ever before. The focus is no longer just on avoiding complications. It’s about living without constant fear, without constant fingersticks, without choosing between insulin and groceries. You don’t have to do it alone. Support groups, diabetes educators, and online communities exist. You’re not broken. You’re adapting. And with the right tools and knowledge, you can live a full life - on your terms.Can type 1 diabetes be prevented?
Currently, there’s no way to prevent type 1 diabetes in most people. It’s an autoimmune condition triggered by genetics and unknown environmental factors. However, teplizumab (Tzield) can delay the onset of clinical type 1 diabetes in people who test positive for multiple autoantibodies and have abnormal blood sugar levels but haven’t yet developed symptoms. This is the first and only FDA-approved intervention to delay progression.
Is insulin the only treatment for type 1 diabetes?
Yes, insulin is essential for survival in type 1 diabetes because the body can’t produce it. No other medications can replace insulin. However, adjunct therapies like pramlintide (an amylin analog) can help with mealtime blood sugar control in some people. New treatments like teplizumab delay disease onset, and stem cell therapies aim to restore insulin production - but none eliminate the need for insulin in established type 1 diabetes.
How often should I check my blood sugar?
If you’re using fingerstick testing, check at least 4-10 times daily - before meals, after meals, at bedtime, and sometimes overnight. If you use a continuous glucose monitor (CGM), you’ll still need to check with a fingerstick if the CGM reading doesn’t match how you feel, or if your device asks for calibration. Most people on CGMs aim to keep their sensor active 24/7 and rely on trends rather than constant fingersticks.
Can I still eat sugar with type 1 diabetes?
Yes. You don’t need to eliminate sugar. The key is matching insulin to the carbs you eat. A cookie or piece of cake is fine if you calculate the carbs and give the right insulin dose. The goal isn’t perfection - it’s balance. Many people with type 1 diabetes enjoy desserts, alcohol, and fast food - they just plan for it.
What happens if I miss an insulin dose?
Missing a dose - especially of long-acting insulin - can cause your blood sugar to rise quickly and lead to diabetic ketoacidosis (DKA), a medical emergency. If you miss a bolus (mealtime) insulin, you may need to correct with a partial dose, depending on your current blood sugar and carb intake. If you miss basal insulin, contact your healthcare provider immediately. Never skip insulin to save money - ask about patient assistance programs. Rationing insulin is dangerous and can be fatal.
Are insulin pumps better than injections?
Pumps aren’t better for everyone - but they’re better for many. They offer more flexibility, reduce the number of daily injections, and with CGM integration, can automatically adjust insulin to prevent highs and lows. Studies show improved time-in-range and lower A1C levels with pumps. But they require training, maintenance, and cost more upfront. Some people prefer the simplicity and lower cost of injections. The best option depends on your lifestyle, budget, and comfort with technology.



Noel Molina Mattinez
November 16, 2025 AT 19:04Just got diagnosed last month and honestly I’m still in shock
They told me I need insulin and I thought they were joking
Now I’m injecting like a pro and my sugar’s under control
Still hate the finger pricks though
Roberta Colombin
November 17, 2025 AT 07:52Thank you for sharing this with such clarity and compassion.
Many people still believe type 1 is caused by sugar or laziness.
This post helps correct those myths with facts and heart.
If you’re new to this diagnosis, know you’re not alone.
There are communities, resources, and people who understand.
You’re not broken. You’re learning. And you will adapt.
Take it one day at a time. You’ve got this.
Dave Feland
November 17, 2025 AT 21:51Let’s be precise: the claim that 'half of new cases occur in adults over 30' is misleadingly vague.
The CDC’s 2021 surveillance data shows only 38.7% of incident T1D cases occurred in individuals aged 30+.
Furthermore, the term 'adult-onset type 1' is a misnomer - it’s LADA (latent autoimmune diabetes in adults), a distinct subtype with slower beta-cell destruction.
Confusing LADA with classic childhood-onset T1D dilutes clinical accuracy.
Also, Tzield’s mechanism is not 'delaying onset' - it’s modulating CD8+ T-cell-mediated destruction via anti-CD3 monoclonal antibody binding.
Stop oversimplifying immunology for clickbait.
Ashley Unknown
November 18, 2025 AT 02:28Okay but have you heard about the government’s secret plan to make everyone diabetic so they can sell insulin at inflated prices?
I mean, why else would they push CGMs and pumps so hard?
And don’t get me started on Big Pharma funding the ADA - they’re literally profiting off our suffering.
My cousin’s friend’s neighbor got diagnosed right after her insurance dropped her coverage - coincidence? I think not.
They want us dependent. They want us scared. They want us paying $300 for a vial of insulin that costs $6 to make.
And now they’re pushing stem cells like it’s magic - but what if it’s just a distraction from the real issue: healthcare capitalism?
I’m not saying it’s a conspiracy - I’m saying it’s systemic.
And don’t tell me to 'just get a pump' - I can’t afford it, and neither can half the people reading this.
Why is no one talking about why insulin is so expensive?
Why are we being sold hope instead of justice?
My blood sugar is 180 right now and I’m crying because I skipped my dose to save money.
And this post? It’s beautiful.
But it’s not enough.
Georgia Green
November 19, 2025 AT 15:58CGM changed my life but I keep forgetting to calibrate
Also carb counting is still so hard I just guess half the time
My pump beeps at 3am and I just want to sleep
But hey at least I’m not in the ER anymore
Thanks for the info though, really helpful
Christina Abellar
November 21, 2025 AT 13:30Thanks for writing this. Clear, accurate, and kind.
People need to hear this.
Eva Vega
November 23, 2025 AT 07:19The pharmacokinetic profiles of rapid-acting analogs (lispro, aspart, glulisine) demonstrate significantly faster absorption and shorter duration than regular human insulin, which is critical for postprandial glucose control in T1D.
Furthermore, the integration of CGM-derived data with predictive low-glucose suspend algorithms in hybrid closed-loop systems has been shown in multiple RCTs to increase time-in-range by 12–15% while reducing hypoglycemic events by 30–40% compared to MDI.
These are not incremental improvements - they represent a paradigm shift in metabolic management.
Matt Wells
November 24, 2025 AT 16:30While the article contains a number of factual inaccuracies - particularly regarding the classification of LADA as type 1 diabetes - its tone is commendably empathetic.
Nevertheless, the omission of any discussion on the limitations of current insulin formulations - such as their inability to replicate the physiological biphasic secretion pattern - renders the piece incomplete.
One must also consider the psychological burden of perpetual glycemic surveillance, which remains under-addressed in mainstream discourse.
Improvement is possible, but only through rigorous scientific literacy, not feel-good narratives.
George Gaitara
November 25, 2025 AT 20:12Everyone’s acting like this is just about blood sugar.
What about the fact that insulin prices went up 300% in 10 years while the cost to produce it dropped?
And why are we being told to 'just use a pump' when most people can’t afford it?
And why is the ADA funded by pharmaceutical companies?
They don’t want you cured - they want you dependent.
They’re selling you a life sentence with a shiny device.
And now they’re pushing stem cells like it’s a miracle - but what if it’s just a way to sell you more stuff?
Don’t believe the hype. This is a business. And you’re the product.
Deepali Singh
November 27, 2025 AT 11:46Statistical analysis of global T1D incidence trends from 2000–2023 reveals a 3.4% annual increase, with the steepest rise observed in high-income countries despite stable genetic prevalence.
This suggests environmental triggers - possibly microbiome disruption or viral epitope mimicry - are accelerating autoimmune beta-cell destruction.
Teplizumab’s efficacy (median delay: 2.5 years) is statistically significant (p<0.001) but clinically modest for individuals already seropositive.
Moreover, the economic burden of CGM utilization, while reducing long-term complications, introduces new financial toxicity through sensor replacement cycles and subscription fees.
Policy interventions must address both biological and socioeconomic dimensions simultaneously - otherwise, therapeutic advances merely exacerbate health inequities.