Antipsychotic Medication Comparison Tool
Select your preferences below to see a recommended antipsychotic medication:
Medical History
Monitoring Preferences
When you or a loved one is diagnosed with schizophrenia, the medication maze can feel overwhelming. One name that often pops up is Clozapine is an atypical antipsychotic reserved for treatment‑resistant schizophrenia (TRS) because of its unique effectiveness and strict safety monitoring. But is it always the best choice? How does it stack up against more commonly prescribed options like Risperidone is a second‑generation antipsychotic known for its relatively mild side‑effect profile and once‑daily dosing or Olanzapine is another atypical drug that delivers strong symptom control but often leads to weight gain? This guide walks you through the key differences, so you can weigh the facts without getting lost in medical jargon.
Key Takeaways
- Clozapine is the gold standard for treatment‑resistant schizophrenia but requires regular blood tests for Agranulocytosis is a dangerous drop in white blood cells that can be fatal if unnoticed.
- Risperidone offers solid efficacy with fewer metabolic side effects, making it a common first‑line option.
- Olanzapine and Quetiapine excel at mood stabilization but carry a higher risk of weight gain and metabolic syndrome.
- Haloperidol remains useful for acute agitation but brings a higher chance of movement disorders.
- Your choice should balance symptom control, side‑effect tolerance, and the level of monitoring you’re comfortable with.
Understanding Clozapine’s Niche
Only about 30% of people with schizophrenia qualify for Treatment‑resistant schizophrenia is a condition where symptoms persist after trials of two adequate antipsychotic regimens. For this group, Clozapine can reduce relapse rates by up to 40% compared to other drugs. The trade‑off? Patients must undergo weekly absolute neutrophil count (ANC) checks for the first six months, then bi‑weekly or monthly thereafter.
Why the intense monitoring? Clozapine’s most feared side effect is Agranulocytosis, which occurs in roughly 0.8% of users but can be caught early with regular blood work. In contrast, most other antipsychotics carry a negligible risk of this condition.
Alternatives At a Glance
Below is a quick snapshot of five widely used antipsychotics that often serve as Clozapine alternatives. Each has its own balance of efficacy, side‑effect risk, and monitoring burden.
| Medication | Efficacy in TRS | Common Side Effects | Monitoring Needed | Weight‑Gain Risk | Cardiac Concerns |
|---|---|---|---|---|---|
| Clozapine | High (gold‑standard) | Sedation, hypersalivation, Agranulocytosis | Weekly ANC (first 6mo), then bi‑weekly/monthly | Low‑moderate | Post‑ural hypotension, myocarditis (rare) |
| Risperidone | Moderate | Prolactin elevation, mild EPS | None beyond routine labs | Low | QTc prolongation (monitor if cardiac history) |
| Olanzapine | High for acute psychosis | Weight gain, drowsiness, metabolic syndrome | Fasting glucose & lipids every 3‑6mo | High | Minimal |
| Quetiapine | Moderate (good for mood symptoms) | Sedation, orthostatic hypotension | None specific | Moderate | Rare QTc issues |
| Haloperidol | Moderate (often used for agitation) | Extrapyramidal symptoms, tardive dyskinesia | None beyond routine labs | Low | QTc prolongation possible |

Side‑Effect Deep Dive
Side effects are the main reason patients switch drugs. Below are the two big safety flags you’ll hear about most often.
- Metabolic syndrome: A cluster of high blood pressure, elevated blood sugar, excess abdominal fat, and abnormal cholesterol. Drugs like Olanzapine and Quetiapine have a Metabolic syndrome is a serious health risk that can lead to diabetes and heart disease incidence as high as 30% after one year.
- Movement disorders: Including Parkinson‑like tremors and tardive dyskinesia. Haloperidol and high‑dose Risperidone are the usual suspects.
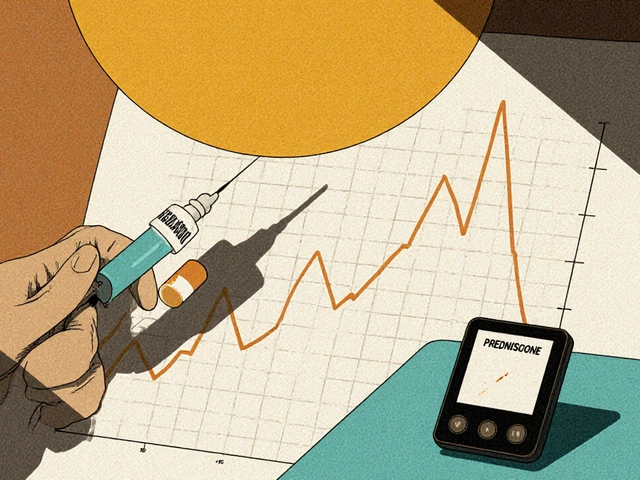
If you’re weighing Clozapine against these alternatives, ask yourself how willing you are to handle regular blood draws in exchange for a lower chance of metabolic issues.
Practical Decision Guide
- Confirm diagnosis: Make sure the patient truly has TRS. A trial of two other atypicals at therapeutic doses for at least six weeks each is the standard benchmark.
- Assess monitoring capacity: Do you have access to a lab that can process ANC results quickly? If not, a drug with less stringent monitoring may be safer.
- Identify side‑effect priorities: Are weight gain and diabetes concerns higher than the hassle of blood work? Choose Olanzapine or Quetiapine. Is sedation a problem? Risperidone might be a better fit. \n
- Consider comorbidities: A history of cardiac disease tilts the scale away from Haloperidol and towards drugs with minimal QTc impact, such as Clozapine (when monitored) or Risperidone.
- Plan for long‑term follow‑up: Regardless of the choice, schedule regular check‑ins for side‑effect screening, weight, glucose, and lipid panels.
Checklist for Patients & Caregivers
- Has a psychiatrist confirmed TRS?
- Do you have reliable access to weekly blood tests?
- Are you comfortable with potential weight gain?
- Any history of heart problems or seizures?
- Do you understand the signs of agranulocytosis (fever, sore throat, fatigue)?
Answering these questions honestly will help you and your doctor land on the medication that feels safest and most effective for you.
Frequently Asked Questions
Why is Clozapine only used after other drugs fail?
Clozapine shows the highest efficacy for treatment‑resistant schizophrenia, but its risk of Agranulocytosis mandates strict blood monitoring. Because of that burden, clinicians reserve it for cases where two other antipsychotics haven’t worked.
Can I switch from Clozapine to another antipsychotic if side effects become intolerable?
Yes, but the switch should be gradual and supervised. A taper over 1‑2 weeks helps reduce withdrawal psychosis, and the new medication will need its own titration schedule.
How often do I need blood tests on Clozapine after the first six months?
After the initial 6‑month intensive phase (weekly), the schedule drops to bi‑weekly for months7‑12, then monthly for stable patients.
Is Risperidone safe for people with a history of high prolactin levels?
Risperidone can raise prolactin further, so patients with pre‑existing hyperprolactinemia may need an alternative like Olanzapine or a partial dopamine agonist.
What lifestyle changes help counteract weight gain from Olanzapine?
Regular aerobic exercise (150min/week), a low‑glycemic diet, and routine metabolic screening can blunt the weight‑gain curve. Some clinicians add metformin to mitigate insulin resistance.





Julie Gray
September 29, 2025 AT 02:46In light of the prevailing pharmacological agenda, it is evident that Clozapine’s mandated hematologic surveillance serves not merely a clinical purpose but also functions as a mechanism of population control, ensuring that only those who acquiesce to continuous laboratory oversight remain on the regimen.
Lisa Emilie Ness
October 8, 2025 AT 06:41Clozapine works but the blood tests are a hassle
Emily Wagner
October 17, 2025 AT 10:35The dialectic of efficacy versus safety in antipsychotic selection mirrors the age‑old tension between freedom and security; Clozapine offers unparalleled potency for treatment‑resistant cases, yet its hematologic demands impose a custodial vigilance that reshapes the therapeutic contract.
Mark French
October 26, 2025 AT 13:29I understand the anxiety that comes with weekly blood draws; many patients feel definately apprehensive, yet the data shows that early detection of agranulocytosis dramatically reduces mortality, and that trade‑off often justifies the inconvenience.
Daylon Knight
November 4, 2025 AT 17:24Oh great another drug that needs you to swing by the lab more often than you visit the grocery store – because who doesn’t love extra paperwork?
Jason Layne
November 13, 2025 AT 21:18The pharmaceutical consortium deliberately obscures the true risk profile of Clozapine, presenting it as the “gold standard” while quietly ensuring that the requisite weekly ANC tests keep patients tethered to a surveillance infrastructure that benefits insurance algorithms more than individual health. They exploit the rarity of agranulocytosis to justify invasive monitoring, turning a therapeutic necessity into a data‑harvesting operation. This calculated opacity forces clinicians into a compliance loop that privileges market control over patient autonomy.
Hannah Seo
November 23, 2025 AT 01:12For anyone weighing Clozapine against alternatives, consider a stepwise approach: confirm treatment‑resistance with two trials, verify access to reliable labs, and discuss the relative metabolic profiles of Olanzapine and Quetiapine. If weight gain is a primary concern, Risperidone may be preferable, whereas Clozapine remains unmatched for refractory psychosis when you can commit to regular monitoring.
Victoria Unikel
December 2, 2025 AT 05:07Honestly i feel kinda drained just thinking about all those meds – the side effects list reads like a nightmare, and the constant blood work just adds to the gloom.
Lindsey Crowe
December 11, 2025 AT 09:01Sure, because adding another drug to the mix always solves everything.
Rama Hoetzlein
December 20, 2025 AT 12:56The modern psychopharmacology landscape is a labyrinthine theater where clinicians perform a delicate balancing act between efficacy and iatrogenic harm, and Clozapine occupies the gilded throne of this tragic drama. Its unparalleled potency in treatment‑resistant schizophrenia is a fact that cannot be dismissed, yet the surrounding discourse is often clouded by an obsessive reverence that borders on cult worship 😒. Proponents trumpet its superior relapse reduction rates while conveniently glossing over the morbidity associated with agranulocytosis, a condition that, despite its low incidence, carries a mortality risk that rivals that of many oncologic therapies 😱. The mandated weekly absolute neutrophil counts (ANC) for the first six months constitute a logistical burden that many patients cannot meet, especially in underserved regions where laboratory infrastructure is sparse. Moreover, the metabolic side‑effect profile of Clozapine, though comparatively moderate, still predisposes a subset of patients to weight gain and dyslipidemia, further complicating long‑term management. In contrast, risperidone offers a modest efficacy with a benign metabolic footprint, making it a pragmatic first‑line option for those wary of intensive monitoring. Olanzapine, while effective, brings a high propensity for weight gain and insulin resistance, demanding regular glucose and lipid assessments that echo Clozapine’s monitoring demands albeit with different parameters. Quetiapine’s sedative properties can be advantageous in comorbid insomnia, yet its orthostatic hypotension risk necessitates careful titration. Haloperidol, the archetype of typical antipsychotics, remains valuable for acute agitation but is marred by extrapyramidal symptoms that can be debilitating. The decision matrix therefore should be individualized, weighing the severity of psychosis against the patient’s capacity for adherence, comorbid conditions, and access to healthcare resources. Ignoring these variables in favor of a one‑size‑fits‑all narrative is intellectually lazy and clinically irresponsible. When clinicians succumb to the allure of “gold‑standard” rhetoric without scrutinizing the practicalities, they betray the very patients they aim to serve. A judicious approach involves shared decision‑making, transparent discussion of risks, and contingency plans for monitoring failures. Ultimately, Clozapine’s role is irreplaceable for a minority of patients, but it should never eclipse the nuanced evaluation required for optimal antipsychotic stewardship 🙄. Clinicians must also remain vigilant for emerging data that could shift current hierarchies of treatment.
Lorena Garcia
December 29, 2025 AT 16:50I think the key is to match the medication to the person’s lifestyle – if weekly labs feel like a mountain, exploring risperidone or olanzapine first can keep treatment moving while still addressing symptoms.
Joe Evans
January 7, 2026 AT 20:44Great summary! 😊, I love how you laid out the pros and cons, especially the clear bullet‑point style, which makes it easy to compare options, and remember to check weight and blood work regularly! 👍, Keep the info coming! 🎉
Sharon Cohen
January 17, 2026 AT 00:39Everyone seems to glorify Clozapine, but I’d rather stick with a drug that doesn’t turn my blood work into a weekly drama.
Rebecca Mikell
January 26, 2026 AT 01:46Thanks for the thorough breakdown; it really helps to see the trade‑offs side by side, and I’ll bring these points to my next appointment.